BIMONTHLY INTERNAL ASSESSMENT FOR THE MONTH OF JANUARY 2021
26 year old woman with complaints of altered sensorium since 1 day,headache since 8 days,fever and vomitings since 4 days
More here: https://harikachindam7.
Case presentation links:
https://youtu.be/fz9Jssoc-mA
https://youtu.be/d4lLX04oL8s
https://youtu.be/CSCxw2zp7Oc
a). What is the problem representation of this patient and what is the anatomical localization for her current problem based on the clinical findings?
- 26 year old female married 10yrs back mother of 2 children tailor & agricultural labourer by occupation presented to casualty in a state of altered sensorium & irrelevant talk
- History of B/L hand small joint pains 6 yrs back Multiple joint pains 3 yrs back and diagnosed as SLE and using treatment which she stopped 10 days ago.
- C/o headache since 1 month which increased in last 10 - 15 days associated with vomitings since 1 week and fever, neck pain , generalized weakness since 4 days and altered sensorium with irrelevant talk since 1 day.
- Diagnosed as TB meningitis
1) KIDNEYS: Hyponatremia secondary to SIADH.
2) BRAIN: TB meningitis , Acute infarct in left thalamus.
b) What is the etiology of the current problem and how would you as a member of the treating team arrive at a diagnosis? Please chart out the sequence of events timeline between the manifestations of each of her problems and current outcomes.
1) Hyponatremia.
2) Euvolemic Hyponatremia ( as there was no signs of fluid overload or hypotension) secondary to SIADH.(SIADH secondary to TUBERCULAR MENINGITIS).
3) TUBERCULAR MENINGITIS. ( CSF cbnaat came positive and also cell count revealed lymphocytosis,with low glucose and chloride and increased CSF protein. - evident of TB meningitis.
4) ACUTE INFARCT IN LEFT THALAMUS (secondary to vasculitis).
Sequence of events:
2010: marriage
!
2011: 1st child birth (male)
!
2012: 2nd child birth (female)
!
2014: Both hands small joints pain progressed to elbow and shoulder - relieved with treatment @ local RMP
!
2017: Multiple joint pains - diagnosed as SLE & started on treatment
!
2020 (december): - headache on& off 1-2 times/week relieved with treatment
!
Increased headache from 15 days
!
10 days back stopped methyl prednisolone
!
vomitings from 1 week
!
Fever, neckpain, generalized weakness & decreased appetite from 4 days
!
Admitted to a local hospital and @ night went to bathroom and fell down in a state of altered sensorium
!
Same day presented to our casualty @ around
3 am in a state of altered sensorium & irrelevant speech
c) What is the efficacy of each of the drugs listed in her prior treatment plan that she was following since last two years before she stopped it two weeks back?
Patient was on medication for SLE (Hydrochloroquine-200mg/OD,Sulfasalazine,Methylprednisolone,Alandronic acid and Cholecalciferol,Aceclofenac,Flupirtine,Gabapentine,Methylcobalamin tablets), which she stopped 10 days back.
https://pubmed.ncbi.nlm.nih.gov/8815753/HCQ therapy is effective on clinical improvement of SLE patients through interfering with inflammatory signaling pathways, reducing anti-DNA autoantibodies and normalizing the complement activity.
https://pubmed.ncbi.nlm.nih.gov/29987550/#:~:text=Conclusion%3A%20HCQ%20therapy%20is%20effective,and%20normalizing%20the%20complement%20activity
Why was she given bisphosphonates?
What is the efficacy of using primary bisphosphonate prophylaxis for patients started on corticosteroids?
Why was she given bisphosphonates?
What is the efficacy of using primary bisphosphonate prophylaxis for patients started on corticosteroids?
Bisphosphonates reduce the risk of vertebral fractures and the prevention and treatment of steroid‐induced bone loss.
What is the efficacy of using primary PPI prophylaxis during initiation of any corticosteroids to prevent Gi ulcers?
It is a common practice to co-prescribe PPI alongside glucocorticoid therapy, to taper the theoretical risk of peptic ulcer associated with glucocorticoid therapy. However, peptic ulcer is a rare complication of systemic glucocorticoid therapy and occurs in less than 0.4–1.8% of patients. With such low risks, there is no indication for routine prophylaxis with PPIs in this situation.
http://www.esim.eg.net/article.asp?issn=1110-7782;year=2018;volume=30;issue=3;spage=173;epage=174;aulast=Agarwal
https://pubmed.ncbi.nlm.nih.gov/23657097/
https://pubmed.ncbi.nlm.nih.gov/23657097/
d) Please share any reports around similar patients with SLE and TB meningitis?
https://link.springer.com/article/10.1007/s10067-020-04940-9
https://www.ijidonline.com/article/S1201-9712(14)01177-1/fulltext
Any reports of normal csf leukocyte count and normal csf protein in meningitis?
https://www.ijidonline.com/article/S1201-9712(14)01177-1/fulltext
Any reports of normal csf leukocyte count and normal csf protein in meningitis?
What could be the probable cause for a normal csf leukocyte count in a patient with chronic meningitis?
Meningitis in the absence of pleocytosis on CSF is rare. If this occurs, causative organism is likely bacterial.
https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-019-4204-z
e) What is the sensitivity and specificity of ANA in the diagnosis of SLE?
e) What is the sensitivity and specificity of ANA in the diagnosis of SLE?
The prevalence of ANA at a titer of ≥1:80 and ≥ 1:160 was 8% and 4%, respectively, in HC; and it was 12% and 6% respectively, in MMP patients. The prevalence of anti-dsDNA was 0% in HC and 3% in MMP patients. When using HC sera for the diagnosis of SLE, the sensitivity of ANA at a titer of ≥ 1:80 and ≥ 1:160 was 98% and 90%, respectively, with specificity of 92% and 96%, respectively. The specificity decreased to 88% and 94%, respectively, when using sera from MMP patients. The specificity of anti-dsDNA was 100% and 97%, when using sera from HC and MMP patients, respectively.
https://pubmed.ncbi.nlm.nih.gov/24383972/
2) Please go through the two thesis presentations below and answer the questions below by also discussing them with the presenters:
A) https://youtu.be/sw8o8y5Yw_I
What was the research question in the above thesis presentation?
Association of serum magnesium with type-2 diabetes mellitus
What was the researcher's hypothesis?
2) Please go through the two thesis presentations below and answer the questions below by also discussing them with the presenters:
A) https://youtu.be/sw8o8y5Yw_I
What was the research question in the above thesis presentation?
Association of serum magnesium with type-2 diabetes mellitus
What was the researcher's hypothesis?
Hypomagnesemia in diabetes was associated with poorer glycemic control, retinopathy, nephropathy, and foot ulcers.
What is the current available evidence for magnesium deficiency leading to poorer outcomes in patients with diabetes?
What is the current available evidence for magnesium deficiency leading to poorer outcomes in patients with diabetes?
Hypomagnesemia in diabetes was associated with poorer glycemic control, retinopathy, nephropathy, and foot ulcers.
B) https://youtu.be/jXVS5J1-RNE
What was the research question in the above thesis presentation?
24 hrs urinary sodium excretion values in newly diagnosed hypertensive patients.
What was the research question in the above thesis presentation?
24 hrs urinary sodium excretion values in newly diagnosed hypertensive patients.
What was the researcher's hypothesis?
Low level of urinary sodium excretion related to low rate of hypertension and slower BP increase with age and better prognosis.
What is the current available evidence for the utility of monitoring salt excretion in the hypertensive population?
What is the current available evidence for the utility of monitoring salt excretion in the hypertensive population?
Low level of urinary sodium excretion related to low rate of hypertension and slower BP increase with age.
https://bmccardiovascdisord.biomedcentral.com/articles/10.1186/s12872-018-0787-3#:~:text=High%20dietary%20salt%20increases%20BP,high%20dietary%20salt%20%5B13%5D.
3) Please critically appraise the full text article linked below:
https://onlinelibrary.wiley.
What is the efficacy of aspirin in stroke in your assessment of the evidence provided in the article. Please go through the RCT CASP checklist here https://casp-uk.net/casp-
https://bmccardiovascdisord.biomedcentral.com/articles/10.1186/s12872-018-0787-3#:~:text=High%20dietary%20salt%20increases%20BP,high%20dietary%20salt%20%5B13%5D.
3) Please critically appraise the full text article linked below:
https://onlinelibrary.wiley.
What is the efficacy of aspirin in stroke in your assessment of the evidence provided in the article. Please go through the RCT CASP checklist here https://casp-uk.net/casp-
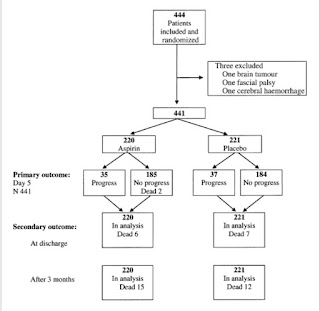
The main results of the trial showed that aspirin treatment did not significantly reduce the rate of stroke progression. The progression rate was 15.9% amongst patients treated with aspirin and 16.7% for those on placebo.
The ability to live at home, to walk unaided, or need for further institutionalized care after discharge was not significantly improved in the aspirin group .
RCT CASP checklist:
https://documentcloud.adobe.com/link/review?uri=urn:aaid:scds:US:8d251179-8d1c-435c-803e-0daf96229a3f
4) Please mention your individual learning experiences from this month.
4) Please mention your individual learning experiences from this month.
- Iron deficiency leading to pancytopenia
- Renogram and criteria for renal transplant
- Management of resistant hypertension jn CKD by adjusting the dosing and dosage of drugs
- Wet beri beri
- Hypothyroidism and kidney failure
- A case of pleuro peritoneal connections secondary to liver abscess
- CLD with portal HTN secondary to ? HCV/Alcohol
- AKI on CKD secondary to Urosepsis
- Pericardiocentesis
- Pleural tap
- TB meningitis
5) a) What are the possible reasons for the 36 year old man's hypertension and CAD described in the link below since three years?
https://vamsikrishna1996.
https://vamsikrishna1996.
b) Please describe the ECG changes and correlate them with the patient's current diagnosis.
Rythm - Initial ecgs rate is Irregular with VPC ,later becoming regular
Axis - Normal
VPCs followed by a compensatory pause
QS complexes in v1 - v3Poor R wave progression
T-wave inversions in v4 - v6
Mild ST segment elevation in v1 - v4
c) Share an RCT that provides evidence for the efficacy of primary PTCA in acute myocardial infarction over medical management. Describe the efficacy in a PICO format.
P
214 patients with stable angina, normal ventricular function and a proximal stenosis of the left anterior descending coronary artery > 80%
I
Balloon angioplasty
Medical therapy alone
C
Balloon angioplasty (n = 72)
Medical therapy alone (n = 72)
O
At an average follow-up period of 3 years
p = 0.28, angioplasty vs. medical treatment
There was no difference in mortality or infarction rates among the groups



Comments
Post a Comment