SHORT CASE-1
A 50 years old male, mason by occupation and resident of Bhongir, came to the hospital with chief complaints of fever since 2 months, and loss of appetite since 2 months.
History of presenting illness
A 50-year-old mason who was happily living with his family daily wakes up at 5 am, goes for a walk to get milk, and returns home. He then has tea with biscuits and rice for breakfast, then leaves for his work by 9 am. He has rice, for lunch, with curries at his workplace. He comes back from work at either 7 or 8 pm. He has rice for dinner at 9 pm and goes to sleep by 10 pm.
2 months back while he was working he felt generalized weakness & body pains for which he left work early and went to home. The next day morning he had fever for which he bought some tablets from a local pharmacy.
2 days later he was taken to a local ayurvedic by his family members on suspicion of jaundice where he was given some herbal medicine 3 doses (1 dose/week) and advised of some dietary restrictions.
Even after 3 weeks, his fever doesn't come down and he felt no change in his general condition.
He also lost his appetite gradually since 2 months, and history of weight loss since 2 months.
Since 20 days, his fever increased usually more in the evenings which would continue the whole night, and reduce by morning, and is associated with chills for which he was brought to our hospital.
Patient also complained of on & off pain in the abdomen in the umbilical and right lumbar region, which was insidious in onset, gradually progressive, non-radiating, aggravated while walking (around 100 meters), and relieved on rest.
H/o burning micturition present
No h/o urgency, frequency, incontinence, polyuria, polydipsia, nocturia, or urethral discharge.
No h/o sore throat, cough, or cold
No h/o vomiting, diarrhea
No h/o rash over the body, bleeding gums, Malena
No h/o headache, photophobia, involuntary movements, altered behavior
No H/o pedal edema, SOB, chest palpitations, chest pain, and tightness.
Past History
Patient is a known case of pulmonary tuberculosis 25 years ago, for which he used ATT for 6 months.
Not a known case of DM, HTN, CVA, CAD, thyroid disorders, asthma, and epilepsy.
Personal history
Diet - mixed
Appetite - decreased since 2 month
Bowel & Bladder habits: Regular
Sleep - decreased
Addictions - 90 ml occasionally since 35 years.
Family history
No similar complaints
Surgical history
Appendicectomy was done 30 years ago
General examination
Examination was done in a well-lighted room, with consent and informing the patient in the presence of a female attendant.
Patient was conscious, coherent, and cooperative, well oriented to time, place, and person.
Pallor - present
Icterus- absent
Cyanosis- absent
Clubbing - absent
Lymphadenopathy- absent
Pedal edema - absent
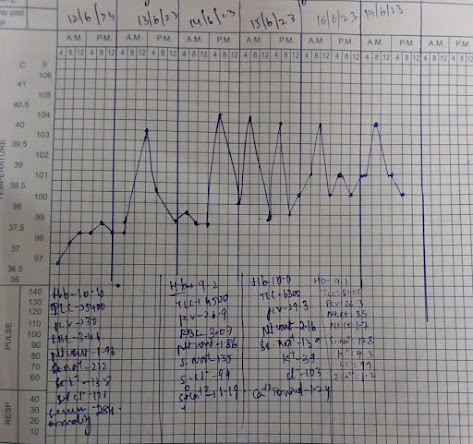
Vitals
Temperature- 38⁰ C
PR - 105bpm
RR - 23 CPM
BP - 100/60 mmHg
SpO2 - 99% at RA
GRBS - 114mg/dl
SYSTEMIC EXAMINATION
RESPIRATORY SYSTEM
Patient examined in the sitting position
Inspection
Lips and tongue normal
Oral candida - absent
Poor oral hygiene
Trachea appears to be central
Shape appears to be elliptical, B/L symmetrical
Mild wasting seen on right side supra scapular & infrascapular region
Respiratory movements appear equal on both sides and abdominothoracic type
No scars, sinuses, and dilated veins.
No lumps and Lesions
No intercostal recession
Palpation
All inspectory findings are confirmed
Apical impulse felt at 5th intercostal space and at the midclavicular line
Total circumference - 34 inches
Hemithorax, Right - 17 inches Left - 17 inches
Anterior Posterior - 8 inches
Transverse - 12 inches
Chest expansion - 2 cms
Tactile vocal fremitus - Right Left
Supraclavicular -. increased normal
Infraclavicular- increased. normal
Mammary- increased normal
Axillary- normal normal
Infra axillary- normal normal
Suprascapular- normal normal
Interscapular- normal normal
Infrascapular- normal normal
Percussion
Resonant in all regions
Auscultation
Fine crepitations were heard in the infraclavicular area.
Normal vesicular breath sounds in other areas.
Vocal Resonance - Right Left
Supraclavicular - increased normal
Infraclavicular- increased normal
Mammary- increased normal
Axillary- normal normal
Infra axillary- normal normal
Suprascapular- normal normal
Interscapular- normal normal
Infrascapular- normal normal
ABDOMINAL EXAMINATION
Inspection
Shape - scaphoid
Umbilicus- centralized, inverted
Scar present of appendicectomy
No dilated veins
No visible pulsations or peristalsis
Palpation:
Soft, tenderness present in epigastrium & hypogastrium
Deep palpation-
No organomegaly
Percussion:
No fluid thrill
Liver span 12 cms
Auscultation:
No bowel sounds heard
CVS EXAMINATION
Inspection:
Shape of the chest- elliptical
No engorged veins, scars, visible pulsations
Palpation:
Apex beat can be palpable in the 5th intercostal space
Auscultation:
S1,S2 are heard
No murmurs
CNS EXAMINATION
Higher mental functions: intact
Cranial nerves intact
Motor examination: R L
Bulk. N N
Tone. N N
Power. N N
Reflexes:
Biceps. 2+ 2+
Triceps. 2+ 2+
Supinator 2+. 2+
Knee 2+.2+.
Ankle. 2+. 2+
Sensory examination: Normal
No meningeal signs
Investigations
Hemogram:
Hb - 10g/dl
PCV -29.3 vol%
Total leucocyte count - 6,300cells/cumm
RBC -3.08millions/cumm
Platelets-2.16lakhs/cumm
Serum electrolytes:
Sodium-134mEq/l
Potassium-3.9mEq/l
Chloride-103mEq/l
RFT:
Creatinine-1.2mg/dl
Urea -41mg/dl
LFT:
Total bilirubin-1.26mg/dl
Direct bilirubin-0.30mg/dl
AST-88IU/L
ALT-72IU/L
ALP-140IU/L
Total proteins-8.3gm/dl
Albumin-2.95gm/dl
RBS-94mg/dl
Serology:
HIV - Reactive
Anti-HCV antibodies -Nonreactive
HbsAg- Non reactive.
USG Abdomen:
Diagnosis:
Denovo Detected RVD + with ? Pulmonary TB reactivation
L2 wedge compression Fracture ? Osteoporotic / Pott's spine
Right upper lobe fibrosis with traction bronchiectasis - old TB sequelae
K/c/o Pulmonary TB 25 yrs ago
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)












.png)

Comments
Post a Comment