THESIS
TOPIC:
PREDICTORS OF OUTCOMES IN PATIENTS WITH PULMONARY ARTERIAL HYPERTENSION AND HEART FAILURE ADMITTED TO A RURAL TERTIARY CARE HOSPITAL
PROBLEM STATEMENT:
HEART FAILURE is one of the leading cause of death at present all over the world.
Inspite of the recent advances and extensive research being done in medical field we are unable to find the exact etiology and predictors of mortality and morbidity in many of the patients with HEART FAILURE and the current mode of treatment is only symptomatic.
In a rural setup with limited resources:
How far we can eliminate the diagnostic and therapeutic uncertainties that persist in a patient with heart failure and what best we can do to improve their outcomes.
INTRODUCTION:
Inspite
of having advancement in field which helps in diagnosing pulmonary
hypertension, it remains the disease that takes lot of time for diagnosis from
the presence of first symptom, many patients are diagnosed only in advanced
stage of disease. 1 Normal pressure in pulmonary artery is 25/10mmHg if the
pulmonary artery pressure exceeds 40/20mmhg or average pressure exceeds 25mmHg,
then the pulmonary hypertension is present. If the pressure in the pulmonary
artery is persistently high then the right ventricle of the heart, from which
the pulmonary artery arises, will not be able to pump properly and then the
symptoms of right heart failure will occur2 .
Pulmonary
artery pressure is increased by many conditions and pulmonary hypertension was
classified accordingly.
Prevalence
of pulmonary artery hypertension of WHO class1 which is caused mainly by
connective tissue disorder, drug, and toxic agents is 15 cases/million adult
population3, 4.
Prevalence
of idiopathic pulmonary artery hypertension 5.9cases/million adult population5,
6, 7, 8 . Pulmonary hypertension due to systemic sclerosis is 7-12% 9, 10
Pulmonary
hypertension due to portal hypertension is 2-16%11, 12
Pulmonary
hypertension due to congenital heart disease is 30%13
Pulmonary
hypertension in sleep apnea is 15-20%14
Heart failure (HF) is one of the most important health
problems in terms of prevalence, morbidity, mortality and health service use.
The prevalence of heart failure in India due to
coronary heart disease, hypertension, obesity, diabetes and rheumatic heart
disease to range from 1.3 to 4.6 million, with an annual incidence of
491600–1.8 million. The actual values
will certainly be higher as
these estimates have
not taken into account
uncommon causes of heart
failure.1
Projections indicate that the prevalence of HF will
increase as much as 46 % from 2012 to 2030.
In brief, HF is a common disease that tend to affect
patients in the most productive years of their lives and result in catastrophic
social and economic consequences with a huge impact on the prognosis and
lifestyle of patients and a growing challenge for health policy makers.
Though chronic
heart failure has been the
subject of interest
among researchers for a
long time, studies
have lately started
focusing on the
entity of ADHF
in view of the
requirement for frequent
hospitalization, the associated
morbidity and mortality and the
resultant burden on health care expenditure. 2-4
Acute decompensated heart failure can be
a disease of new
onset or
due to the
acute worsening of
pre-existing compensated chronic
heart failure. It can
be due to
any etiology such as ischemic,
cardiomyopathic, arrhythmic,
valve dysfunctional, high
output, etc. Based
on the pathophysiology, it
is of two
types, viz. heart
failure with depressed
systolic function and heart
failure with preserved
systolic function.8,9
Inspite of the recent advances and extensive research being done in
medical field we are unable to find the exact etiology and predictors of
mortality and morbidity in many of the patients with heart failure and the
current mode of treatment is only symptomatic.
ADHERE and OPTIMIZE-HF which are registry-based retrospective
studies have identified various
predictors of in-hospital
mortality among such
patients as well as
have devised risk stratification nomograms that are validated.5,6These
studies are superior to pre-designed clinical trials which include carefully
selected patients and whose results cannot be effectively applied in routine
clinical practice. There are sporadic reports that have studied the aetiology
of congestive cardiac failure and precipitating factors of ADHF in Indian
patients admitted in Indian hospitals18,19 .
AIM:
To identify the predictors of outcomes in
patients admitted to a rural
tertiary care hospital with
pulmonary arterial hypertension and heart failure.
OBJECTIVES:
To assess various clinical and investigational
characteristics of patients in relation to their outcomes (morbidity &
mortality)
To analyse if those characteristics has significant
association with outcomes
(morbidity & mortality).
REVIEW OF LITERATURE:
HEART FAILURE is not only a disease of
cardiovascular system per se, but also involves other systems with resultant
signs and symptoms.
They
are:
Cardiopulmonary
connections In the form of exercise intolerance, dyspnea, orthopnea and
paroxysmal nocturnal dyspnea.
Cardiorenal
connections In the form of salt and water retention, edema and anasarca.
Cardioneural
connections In the form of sleep apnea and Chyne-Stokes respiration.
Cardiometabolic
connections In the form of cardiac cachexia.
Heart
failure can be of acute or chronic. It can be due to any aetiology such as
ischemic, cardiomyopathic, arrhythmic, valve dysfunctional, high output, etc.
Based
on the pathophysiology, it is of two types, viz. heart failure with reduced
systolic function and heart failure with preserved systolic function.
Epidemiology
The
epidemiological statistics of heart failure in India is largely an estimate
derived from the scantily available clinical materials, related population
studies and extrapolation of western data. This poor state is due to the
absence of proper surveillance programs for monitoring the trend of heart
failure, and its morbidity and mortality in India. The estimated prevalence of
heart failure in India due to several causes is 1.3 - 4.6 million and its
annual incidence is 0.4 – 1.8 million. The reasons for these higher figures
appear to be the ill effects of industrialization, continuing prevalence of
rheumatic heart disease, restricted access to health care facilities, and
growing size of old age population1 .
The
rough estimate of prevalence of heart failure in India due to coronary artery
disease alone is 0.3 – 1.75 million. The calculated prevalence of heart failure
in India due to hypertension alone ranges from 0.3 million to 1.8 million after
taking into account the results of Hypertension Optimal 17 Treatment trial and
United Kingdom Prospective Diabetes Study trial. Similar presumptive estimation
has found out that the prevalence of heart failure in India due to obesity
alone will be around 0.45 – 0.75 million and that due to diabetes alone will be
around 0.18 million1 .
The
prevalence and incidence of heart failure in India due to other diseases (such
as rheumatic heart disease, infective endocarditis, tuberculous constrictive
pericarditis, idiopathic dilated cardiomyopathy, endomyocardial fibrosis,
etc.), restricted access to healthcare, and low economic status could not be
estimated due to lack of relevant epidemiological data1 .
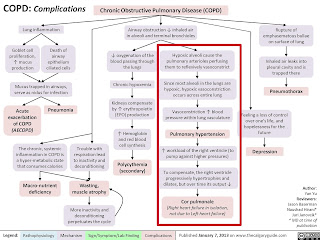
Pathogenesis
Heart
failure is a progressive disorder. It gets started when events such as
myocardial infarction damages the functioning myocytes of heart muscle
resulting in their loss or when events such as unstable hemodynamic forces
disrupt the myocardial cells from generating force, leading on to abnormal
cardiac contraction. The initiating agent for this progressive disorder can be
either abrupt onset (such as in case of acute coronary syndrome) or gradual and
insidious one (such as in case of various overload states). Irrespective of the
nature of insulting event, the final result of the pathological processes that
follow will be the same in the form of a declined pumping capacity of the
cardiac chambers20 .
In
general, patients do not develop the overt symptoms of heart failure as soon as
the damage process sets in. They, for a significant period of time, will either
be totally asymptomatic or might have minimal symptoms on occasions of
exertion. The reasons are unclear yet, but the possible explanation is that
several compensatory mechanisms get activated once the injury occurs and that
those will play a crucial role in modulating the myocardium to function within
the normal physiological range despite its injury, thereby preventing the
failure symptoms. It is when such a prolonged continuous activation of
compensatory processes of these various cytokines and neurohormonal systems
lead on to myocardial remodelling by causing end organ changes within the myocytes,
patients become symptomatic with their heart failure20 .
During
the evolution of asymptomatic heart failure to symptomatic heart failure,
adaptations and consequent mal-adaptations occur at various levels ranging from
metabolic to physiologic to molecular levels22 .
Molecular
adaptations and mal-adaptations
Molecular
level changes are important and seem to play a pivotal role especially in
hereditary idiopathic dilated cardiomyopathies. Though a clear and complete
knowledge is lacking, the molecular response changes are prominently observed
in actin, myosin (especially beta myosin heavy chain), troponin T, other
cytoskeletal proteins, and in functional proteins as well such 19 as calcium
flux proteins, ion channel proteins, excitation-contraction coupling proteins,
etc22,23 .
Metabolic
adaptations and mal-adaptations
These
include
a.
Less reliance on the more efficient mitochondrial ATP production (due to the
small reserve of phosphorylation capacity in heart muscle)
b.
Decreased regulatory function of ATP
c.
Decreased contraction (dyskinesis) when there is transient ischemia
d.
“Stunning” when the dyskinesis persists after reestablishment of the coronary
flow
e.
“Hibernation” when there is chronic reduction of blood flow
f.
Infarction when the blood flow is compromised completely.
These
various stages of ischemic myocardium are compensated for their loss of
function by the non-ischemic myocardium which in turn gets hypertrophied. When
the hypertrophied myocardium becomes deficient to maintain the stroke volume,
ventricular dilatation occurs as per the Frank Starling’s law. It is noteworthy
to mention that the myocardial utilization of fatty acids and glucose is normal
in failing heart as like in a normal heart. Hence the state of energy starvation
in a failing heart is not due to the 20 decreased supply of energy substrates,
but due to the decreased production and function of ATP22,24 .
It is
not clear that whether there is a decrease in the mass of mitochondria compared
to that of myofibrils in the event of myocardial hypertrophy. Except in large
coronary vessel obstruction and in high metabolic states such as pregnancy, the
effect of mitochondrial dysfunction related energy limitation on the failing
heart is meager. Furthermore, increased reactive oxygen radical production
associated with mitochondrial dysfunction may prove further deterrence to the
struggling myocardium22 .
Physiologic
adaptations and mal-adaptations
They
include autonomic nervous system dysfunction and myocardial receptor dysfunction.
Autonomic nervous system dysfunction is in the form of
a.
Increased peripheral vascular resistance
b.
Defective parasympathetic control over the heart
c.
Altered baroreceptor function
d.
Decreased sympathetic response of the heart to various stimuli
Increased
systemic vascular resistance is brought about by the local hyperactive
vasoconstrictors (such as norepinephrine, endothelin, angiotensin II, etc.) and
by the vascular structural changes which in turn are brought about by impaired
endothelial-assisted vasodilatation and fluid retention25-29 .
During
the early stages of heart failure, the depressed cardiac output and arterial
pressure give rise to a heightened neuroendocrine response resulting in the
activation of sympathetic nervous system and renin-angiotensin-aldosterone
system, and in the increased level of arginine vasopressin. All these
neurohumoral responses lead on to sodium and water retention which in turn
restores the cardiac output and arterial pressure through hypervolemia29. As
the heart failure worsens furthermore, these hemodynamic reflexes get blunted
culminating in abnormal postural change responses and in markedly decreased
heart rate variability which is the hallmark of heart failure and an
independent prognostic factor for cardiac related premature deaths30 .
The
myocytes of the failing heart has also been found to show a decrease in beta
adrenergic receptors and cAMP second messenger system. It is important to note
that there are unclear mechanisms apart from the above in making the failing
heart to show a increasingly blunt response to inotropic stimuli as the heart
failure progresses on31 .
This
observation is particularly significant from the therapeutic point of view as
the heart failure patients are treated with beta agonist drugs such as
dobutamine and antagonist drugs such as beta blockers32 .
There
are several hypotheses for explaining the development of heart failure which is
a progressive disease. They are,
a.
Hemodynamic hypothesis
b.
Neurohumoral hypothesis
c.
Inflammatory hypothesis
d.
Remodeling hypothesis
Hemodynamic
hypothesis
This
is mainly based on the law of Laplace which states that the wall tension of a
cylinder depends on the product of pressure within the cylinder and its radius of
curvature. Here the heart especially the left ventricle is considered to be a
cylinder made of myocardium22 .
T = P
X R
Where
T denotes wall tension in dyn/cm, P denotes pressure in dyn/sq.cm, and R
denotes the radius in cm.
And
there are two fundamental principles governing this hemodynamic hypothesis22.
They
are
a.
Dilation of the ventricles leads directly to an increase in tension on each
muscle fiber.
b. An
increase in wall thickness reduces the tension on any individual muscle fiber.
Therefore, ventricular hypertrophy reduces afterload by distributing tension
among more muscle fibers.
23 The
inner surface of the heart cavities has the highest wall tension. It is also
more vulnerable to ischemia as it has the highest workload. The wall stress is
high in failing heart, so is the afterload. Once dilated, the ventricle is
unable to reduce its radius during contraction. The wall tension or the stress
on the myofibrils of a failing heart keeps on increasing throughout the
ejection due to the reduced ejection fraction, thus adding up to extra
afterload. This is unlike in the normal heart where the wall stress decreases
as the volume decreases. The rate at which the myofibrils shorten is also
reduced, affecting the myocardial performance further in a negative manner. The
facts that the ventricular dilatation eventually leads on to functional mitral
and tricuspid incompetence due to ring expansion and that apoptosis can be
induced by myocardial cells on pathological stretching further contribute to
the heart failure33 .
Myocytes
get hypertrophied in response to pressure overload and get elongated with few
cellular division in response to volume overload34,35. This is accompanied at
the molecular level by alterations in mitochondrial size, changes in collagen
content and structure, and changes in interstitium36,37 .
Neurohumoral
hypothesis
A
plethora of neurohormones are seen elevated in patients with heart failure.
Some of the important ones are norepinephrine, epinephrine, endothelin,
arginine vasopressin, atrial and B-type natriuretic peptides, renin and
angiotensin II, prostaglandins, insulin and cortisol. The main function of
majority of these neurohormones in heart failure is salt and water retention 24
along with vasoconstriction38. Few of them prove to be counter-regulatory as
the case with natriuretic peptides whose primary functions in heart failure are
reductions in right atrial pressure, aldosterone secretion and peripheral
vascular resistance, and enhancement of sodium excretion in urine39 .
Heart
failure results in reduced stroke volume and decreased perfusion pressure which
is sensed by the mechanoceptors situated in carotid sinus, aortic arch and
afferent arterioles of kidney. These mechanoceptors in turn activate the RAAS
system, enhance the sympathetic outflow and release the arginine vasopressin,
all contributing to restore the circulatory integrity38 . However, as the heart
failure worsens, the same factors prove detrimental to the myocardial function
through several mechanisms as mentioned above40 .
The
sympathetic overdrive proves favorable for NYHA class IV heart failure by
improving the cardiac output and perfusion pressure through increasing the
heart rate and myocardial contractility. On the other hand, it becomes
detrimental for NYHA class I-III heart failure by relentless ventricular
remodeling, by increasing systemic venous return through salt and water
retention, and by increasing myocardial oxygen consumption41 .
Inflammatory
hypothesis
Recently,
it has been found that there is a significant association between cardiac
diseases and inflammatory cytokines. They have been demonstrated to be
independent predictors of cardiac failure. Some of them are, 25
a.
Erythrocyte sedimentation rate (ESR)
b. C –
Reactive protein (CRP)
c. Interleukin
6 (IL6)
d.
Tumor necrosis factor – alpha (TNF alpha)
In
chronic heart failure patients with resultant cachexia, TNF alpha level is
elevated in the circulation and is found to be significantly activating the
renin-angiotensin-aldosterone system. Animal studies indicate that
overexpression of TNF alpha leads on to adverse remodelling of myocardium.
Molecular studies have found that TNF alpha is also produced from myocardial
cells, though their primary sources are macrophages and leucocytes. Various
experimental studies have demonstrated that cardiac remodelling, failure and
its related cachexia can be significantly contributed by the inflammatory
cytokines. The inhibitors of such cytokines have been found to alter the course
of heart failure in animals, but not in humans42-44 .
Though
still investigational, the role of oxidative stress and reactive oxygen species
in development of heart failure is a potential area of interest. The oxidant
stress pathways in response to chronic exposure to reactive oxygen radicals
damage the myocardium through lipid peroxidation, DNA breakage and cellular
enzymatic changes which in turn culminate in myocyte apoptosis and adverse
myocardial remodeling45 .
Remodeling
hypothesis
The
myocardium exhibits a remarkable plasticity in response to various stimuli and
loading conditions. It responds to various loading conditions by myocardial
hypertrophy and/or myocardial hyperplasia46. In case of hyperplasia of new
myocytes, there is a limitation in their capacity to form and there is a doubt
regarding their functional robustness. Alongside, the process of hyperplasia
also involves the fibroblast producing them in 3:1 to 4:1 ratio with the
myocytes and these fibroblasts replace the lost myocytes during the evolution
of heart failure by producing collagen and other ground substances. Fibrosis is
the major component of myocardial remodeling especially in ischemic
cardiomyopathy. Any pathological change in the myocardial interstitium can also
give rise to both systolic and diastolic dysfunction47 .
Sarcomeres replicate in parallel in pressure hypertrophy, and in parallel and series in volume hypertrophy. The length of sarcomere is fixed and it attains maximum force at 2.2 micrometer. Overstretch of sarcomere is possible but is rare and transient. However, excessive stretch of myocytes results in apoptosis through a locally active mechanism48. Ultimately, certain biochemical changes, altered pattern of excitation-contraction and decreased density of beta adrenoceptors lead to depressed velocity of contraction, attenuated relaxation time and delayed time to peak tension of the myocardium. All these adverse changes give rise to a state of clinical decompensation, thus resulting in heart failure symptoms such as shortness of breath, reduced exercise capacity, etc. Furthermore, the onset and extent of symptoms depend 27 on the severity of onset of overload or injury, level of myocyte loss, level of its replacement by fibrosis, presence or absence of atrioventricular dyssynchrony and heart rate22
BASIC MECHANISMS OF HEART FAILURE
|
SYSTOLIC DYSFUNCTION |
DIASTOLIC DYSFUNCTION |
|
Common in men |
Common in women, obese &
elderly |
|
Normal or low BP |
Usually high BP |
|
S3 gallop |
S4 gallop |
|
Cardiomegaly prominent |
Usually no cardiomegaly |
|
Low EF |
Normal or high EF |
|
Usually coexist with diastolic
dysfunction, especially on exertion |
Mostly exist singly |
|
Treatment well studied and
applied |
Not well studied |
|
Guarded prognosis |
Prognosis not bad |
REVERSIBLE CARDIOMYOPATHIES:
MATERIALS
AND METHODS:
PLACE OF STUDY: Department of General medicine, Kamineni
Institute of Medical Sciences, Narketpally
STUDY PERIOD: November 2020 - October2022
STUDY DESIGN: Prospective
study
SAMPLE SIZE: 50
INCLUSION CRITERIA:
Patients of any gender above or equal to 18yrs of age
at the time of presentation.
Patients Presenting with Pulmonary Arterial Hypertension and Heart failure (New onset or acute worsening of pre
existing chronic heart failure) of any aetiology.
EXCLUSION
CRITERIA:
All confirmed cases of
Patients below 18 years of age (minors)
Patients not capable of giving consent (mentally-ill
patients)
Patients not willing to participate in study
(non-consenting patients)
METHODOLOGY:
A
total of one hundred (n = 50) random patients who were hospitalized for PAH
& HF as well as satisfied our inclusion and exclusion criteria were
selected for the study.
Acute
decompensated heart failure is defined as rapid decompensation of heart
function within a period of one week with resultant signs & symptoms
requiring hospitalization. It could be new onset or worsening of pre-existing
compensated heart failure, and could be of any aetiology (ischemic,
cardiomyopathic, arrhythmic, valve dysfunctional and/or high output). It could
be first time or recurrent admission for ADHF.
Heart
Failure could be systolic failure (with depressed ejection fraction) and/or
diastolic failure (with preserved ejection fraction).
Smoker is
defined as one who has smoked within the previous one year irrespective of
duration of smoking.
NYHA
grading is used to indicate the degree of breathlessness.
Peripheral
edema can be pedal edema or sacral edema or ascites or upper limb
edema or facial puffiness.
New
onset ADHF is defined as the occurrence of acute
decompensation of heart function for the first time in patient’s life. Recurrent
ADHF is defined as any episode of acute decompensation of heart function
that follows a documented first episode at any point in time.
A
patient is said to be Hypertensive if he/she is already on
antihypertensives, and/or if he/she has a high blood pressure documented in the
past, and/or if he/she has a high blood pressure after stabilization of his/her
ADHF, and/or if there are signs of long standing hypertension in fundus, ECG,
chest X-ray and echocardiogram. JNC VIII guidelines are followed for diagnosing
systemic hypertension.
A
patient is said to be Diabetic if he/she is already on OHA or insulin
therapy, and/or if he/she has a high random (>200 mg/dl)/fasting blood sugar
value (>126 mg/dl) or has a high HBA1c value (>6.5%) or has an abnormal
oral glucose tolerance test (>200 mg/dl) documented in the past, and/or if
he/she has a high random/fasting blood sugar (>126 mg/dl) value or has a
high HBA1c value (>6.5%) or has an abnormal oral glucose tolerance test (>200
mg/dl) during hospital stay. The 2021 ADA guidelines are followed for
diagnosing diabetes mellitus.
A
patient is said to have Coronary Artery Disease if he/she is already on
antiplatelet drugs, statins and nitrates, and/or if he/she has coronary artery
disease documented in the past, and/or if he/she has signs of new onset and/or
old coronary artery disease in ECG, Echocardiogram and/or percutaneous coronary
angiogram.
A
patient is said to have Dyslipidemia if he/she is already on
anti-dyslipidemic drugs such as statins, and/or if he/she has high lipid
profile values documented in the past, and/or if he/she is found to have high
fasting lipid profile values on admission.
A
patient is said to have Chronic Kidney Disease if he/she is already on
pharmacological and non-pharmacological measures specific for chronic kidney
disease, and/or if he/she has chronic kidney disease documented in the past,
and/or if he/she is found to have CKD on admission or at 3 month follow up as
per The National Kidney Foundation/Kidney Disease Outcomes Quality Initiative
(NKF/KDOQI) clinical practice guidelines for chronic kidney disease. The
creatinine clearance value is estimated by Cockcroft-Gault formula.
All
cases of heart failure that met my inclusion & exclusion criteria were included
in this study.
History
taking & clinical examination with necessary investigation to assess & analyse various clinical and
investigational characteristics of patients in relation to their outcomes.
Ideal way to diagnose PAH is by right heart catherization,
but in our study we used some of the clinical & investigational
characteristics to diagnose PAH (Pulmonary Arterial Hypertension) after
excluding other possible causes.
Clinical features that are present in patients with
PAH are:
•
Raised
JVP
•
Peripheral
edema
•
Parasternal
heave
•
Palpable
P2
•
RVS3
•
Loud
P2
•
Hepatomegaly
(congestive hepatopathy)
2D ECHO findings that are present in patients with PAH
are:
•
RVSP
> 40 mmhg
•
TR
with PAH
•
Dilated
RA/RV
•
D
shaped LV
ECG finding that are present in patients with
pulmonary hypertension are:
•
P
pulmonale,
•
Right
axis deviation,
•
RV
hypertrophy,
•
RV
strain (ST depression & T wave
inversion in leads corresponding to right ventricle – right precordial leads
V1-V3 +/- V4 & inferior leads II , III , aVF which is often most pronounced
in lead III as this is the most rightward facing lead)
•
Right
bundle branch block,
•
QTc
prolongation
Right ventricular strain pattern has more sensitivity
& specificity compared to right ventricular hypertrophy.in advanced
pulmonary hypertension, supraventricular tachyarrhythmia can occur especially
when the patient has the disease for more than 5 years.1, 43, 51-54.
There may be no change in chest X-ray in PH patients,
but findings that can be present includes:
•
Pruning
that is loss of peripheral blood vessels due to dilation of main pulmonary
artery (prominent pulmonary vasculature).
•
Right
atrium & ventricular hypertrophy is present mainly if there is right heart
failure (RVH on lateral - loss of retrosternal space).
•
Signs
of obstructive airway disease may be present, plural effusion may be present in
few patients1, 43, 55, 56.
INVESTIGATIONS:
Blood sugar
Renal function tests
Lipid profile
Complete blood picture
Chest x-ray PA view
12 lead electrocardiogram
Transthoracic echocardiogram
PROFORMA:
Serial No:
Name:
Age:
Sex:
Occupation:
Address:
IP / OP No:
D.O.A:
D.O.D/D.O.E:
NYHA grade on admission:
Peripheral
edema: Yes/No
Heart rate on
admission:
Systolic blood pressure
on admission:
Etiology:
Ischemic or Non-ischemic
Prior
documented ADHF (Acute
Decompensated Heart Failure):
Yes/No
Smoking: Yes/No
SHT (Systemic Hypertension): Yes/No
DM (Diabetes Mellitus): Yes/No
Dyslipidemia:
Yes/No
CAD (Coronary
Artery Disease): Yes/No
CKD (Chronic Kidney Disease): Yes/No
Blood Urea in mg/dl:
Serum Creatinine in mg/dl:
Serum Sodium in mEq/L:
Hemoglobin in g/dl:
Ejection Fraction:
Outcome:
Asymptomatic/Symptomatically better/Same status/Died
Discharged/LAMA/Referred to higher centre
TABLE NO 1 : DISTRIBUTION OF CASES BASED ON RISK FACTORS (n=50)
|
RISK FACTORS |
PATIENT IMPROVED |
PATIENT MORBID |
PATIENT DIED |
TOTAL |
||
|
NON MODIFIABLE |
AGE (in years) |
18 – 40 |
8 |
5 |
2 |
15 (30%) |
|
41 – 60 |
2 |
15 |
5 |
22 (44%) |
||
|
>60 |
0 |
6 |
7 |
13 (26%) |
||
|
GENDER |
MALE |
9 |
15 |
10 |
34 (68%) |
|
|
FEMALE |
1 |
11 |
4 |
16 (32%) |
||
|
MODIFIABLE |
SMOKING |
1 |
10 |
4 |
15 (30%) |
|
|
ALCOHOL |
8 |
14 |
10 |
31 (62%) |
||
|
DIABETES |
1 |
11 |
3 |
15 (30%) |
||
|
HYPERTENSION |
1 |
10 |
7 |
18 (36%) |
||
|
DYSLIPIDEMIA |
6 |
13 |
9 |
27 (54%) |
||
FIGURE NO 1 : DISTRIBUTION OF CASES
BASED ON RISK FACTORS

TABLE NO 2 : DISTRIBUTION OF CASES BASED
ON ETIOLOGY (n=50)
|
ETIOLOGY |
PATIENT IMPROVED |
PATIENT MORBID |
PATIENT DIED |
TOTAL |
|
WET BERIBERI |
8 |
0 |
0 |
8 (16%) |
|
UNDETERMINED |
1 |
0 |
0 |
1 (2%) |
|
PERIPARTUM CARDIOMYOPATHY |
1 |
0 |
0 |
1 (2%) |
|
HFpEF |
0 |
5 |
1 |
6 (12%) |
|
CAD |
0 |
12 |
5 |
17 (34%) |
|
CKD |
0 |
2 |
4 |
6 12%) |
|
COR PULMONALE |
0 |
4 |
3 |
7 (14%) |
FIGURE NO 2 : DISTRIBUTION OF CASES BASED ON ETIOLOGY

TABLE NO 3 : AGE VERSUS PATIENT
OUTCOME (n=50)
|
AGE IN YEARS |
PATIENT ALIVE n (%) |
PATIENT DIED n (%) |
TOTAL n (%) |
Chi-square χ² |
p VALUE |
OR 95% CI |
|
18 - 40 |
13 (86.7%) |
2 (13.3%) |
15 (30%) |
6.211 |
0.044 |
3.391 (0.655
- 17.556) |
|
41- 60 |
17 (77.3%) |
5 (22.7%) |
22 (44%) |
|||
|
> 60 |
6 (46.2%) |
7 (53.8%) |
13 (26%) |
|||
|
TOTAL n (%) |
36 (72%) |
14 (28%) |
50 |
Of the total 50 patients:
•
15 (30%) were 18 - 40 years of age among which 13 (86.7%) alive
& 2 (13.3%) died.
•
22 (44%) were in between 41 - 60 years of age among which 17
(77.3%) alive & 5 (22.7%) died.
•
13 (26%) were more than 60 years of age among which 6 (46.2%)
alive & 7 (53.8%) died.
•
In our study age has a significant relationship (p 0.044) with
outcomes.
FIGURE NO 3 : AGE WISE PATIENT DISTRIBUTION

FIGURE NO 4 : AGE VERSUS PATIENT OUTCOME

TABLE NO 4 : GENDER VERSUS PATIENT
OUTCOME (n=50)
|
GENDER |
PATIENT ALIVE n (%) |
PATIENT DIED n (%) |
TOTAL n (%) |
Chi-square χ² |
p VALUE |
OR 95% CI |
|
MALE |
24 (70.5%) |
10 (29.5%) |
34 (68%) |
0.105 |
0.745 |
0.80 (0.207
- 3.088) |
|
FEMALE |
12 (75%) |
4 (25%) |
16 (32%) |
|||
|
TOTAL n (%) |
36 (72%) |
14 (28%) |
50 |
Of the total 50 patients:
•
34 (68%) were males among which 24 (70.5%) alive & 10
(29.5%) died.
•
16 (32%) were females among which 12 (75%) alive & 4
(25%) died.
•
In our study gender has no significant relationship (p
0.745) with outcomes.
FIGURE NO 5 : GENDER WISE PATIENT DISTRIBUTION

FIGURE NO 6 : GENDER VERSUS PATIENT OUTCOME

TABLE NO 5 : SMOKING VERSUS PATIENT
OUTCOME (n=50)
|
SMOKING |
PATIENT ALIVE n (%) |
PATIENT DIED n (%) |
TOTAL n (%) |
Chi-square χ² |
p VALUE |
OR 95% CI |
|
SMOKER |
11 (73.3%) |
4 (26.7%) |
15 (30%) |
0.018 |
0.890 |
1.10 (0.283
- 4.282) |
|
NON SMOKER |
25 (72%) |
10 (28%) |
35 (70%) |
|||
|
TOTAL n (%) |
36 (72%) |
14 (28%) |
50 |
Of the total 50 patients:
•
15 (30%) were smokers among which 11 (73.3%) alive & 4
(26.7%) died.
•
35 (70%) were non smokers among which 25 (72%) alive & 10
(28%) died.
•
In our study smoking has no significant relationship (p
0.890) with outcomes.
FIGURE NO 7 : SMOKER VERSUS NON SMOKER

FIGURE NO 8 : SMOKING VERSUS PATIENT OUTCOME

TABLE NO 6 : ALCOHOL VERSUS PATIENT
OUTCOME (n=50)
|
ALCOHOL |
PATIENT ALIVE n (%) |
PATIENT DIED n (%) |
TOTAL n (%) |
Chi-square χ² |
p VALUE |
OR 95% CI |
|
ALCOHOLIC |
21 (67.7%) |
10 (32.3%) |
31 (62%) |
0.733 |
0.391 |
0.56 (0.147
- 2.129) |
|
NON ALCOHOLIC |
15 (79%) |
4 (21%) |
19 (38%) |
|||
|
TOTAL n (%) |
36 (72%) |
14 (28%) |
50 |
Of the total 50 patients:
•
31 (62%) were alcoholics among which 21 (67.7%) alive &
10 (32.3%) died.
•
19 (38%) were non alcoholics among which 15 (79%) alive &
4 (21%) died.
•
In our study smoking has no significant relationship (p
0.391) with outcomes.
•
Of the 21 patients who were alive in alcoholic group 8
patients (38%) improved completely and those were the patients presented with
wet beriberi due to Thiamine deficiency.
FIGURE NO 9 : ALCOHOLIC VERSUS NON ALCOHOLIC

FIGURE NO 10 : ALCOHOL VERSUS PATIENT OUTCOME

TABLE NO 7 : NYHA CLASS VERSUS
PATIENT OUTCOME (n=50)
|
NYHA |
PATIENT ALIVE n (%) |
PATIENT DIED n (%) |
TOTAL n (%) |
Chi-square χ² |
p VALUE |
OR 95% CI |
|
CLASS 4 |
8 (50%) |
8 (50%) |
16 (32%) |
6.239 |
0.044 |
10.00 (1.026
- 97.50) |
|
CLASS 3 |
18 (78.2%) |
5 (21.8%) |
23 (46%) |
|||
|
CLASS 2 |
10 (90.8%) |
1 (9.2%) |
11 (22%) |
|||
|
TOTAL n (%) |
36 (72%) |
14 (28%) |
50 |
Of the total 50 patients:
•
16 (32%) presented with NYHA class 4 SOB among which 8 (50%)
alive & 8 (50%) died.23 (46%) presented with NYHA class 3 SOB among which
18 (78.2%) alive & 5 (21.8%) died.11 (22%) presented with NYHA class 2 SOB
among which 10 (90.8%) alive & 1 (9.2%) died.
•
In our study NYHA classification has significant relationship
(p 0.044) with outcomes.
FIGURE NO 11 : DISTRIBUTION OF PATIENTS BASED ON NYHA GRADE

FIGURE NO 12 : NYHA GRADE VERSUS PATIENT OUTCOME

TABLE NO 8 : PERIPHERAL EDEMA VERSUS
PATIENT OUTCOME (n=50)
|
PERIPHERAL EDEMA |
PATIENT ALIVE n (%) |
PATIENT DIED n (%) |
TOTAL n (%) |
Chi-square χ² |
p VALUE |
OR 95% CI |
|
PRESENT |
28 (75.7%) |
9 (24.3%) |
37 (74%) |
0.953 |
0.328 |
1.944 (0.506
- 7.473) |
|
ABSENT |
8 (61.6%) |
5 (38.4%) |
13 (26%) |
|||
|
TOTAL n (%) |
36 (72%) |
14 (28%) |
50 |
Of the total 50 patients:
•
37 (74%) presented with peripheral edema among which 28
(75.7%) alive & 9 (24.3%) died.
•
13 (26%) had no peripheral edema among which 8 (61.6%) alive
& 5 (38.4%) died.
•
In our study pedal edema has no significant relationship (p
0.328) with outcomes.
FIGURE NO 13 : DISTRIBUTION OF PATIENTS BASED ON PERIPHERAL EDEMA

FIGURE NO 14 : PERIPHERAL EDEMA VERSUS PATIENT OUTCOME

TABLE NO 9 : PRIOR ADHF VERSUS
PATIENT OUTCOME (n=50)
|
ADHF |
PATIENT ALIVE n (%) |
PATIENT DIED n (%) |
TOTAL n (%) |
Chi-square χ² |
p VALUE |
OR 95% CI |
|
RECURRENT |
13 (86.7%) |
2 (13.3%) |
15 (30%) |
2.286 |
0.130 |
3.391 (0.655
- 7.556) |
|
FIRST TIME |
23 (65.7%) |
12 (34.3%) |
35 (70%) |
|||
|
TOTAL n (%) |
36 (72%) |
14 (28%) |
50 |
Of the total 50 patients:
•
15 (30%) had recurrent ADHF among which 13 (86.7%) alive
& 2 (13.3%) died.
•
35 (70%) had symptoms for the first time among which 23
(65.7%) alive & 12 (34.3%) died.
•
In our study recurrent ADHF has no significant relationship (p
0.130) with outcomes.
FIGURE NO 15 : ADHF RECURRENT VERSUS FIRST TIME

FIGURE NO 16 : ADHF VERSUS PATIENT OUTCOME

TABLE NO 10 : CAD VERSUS PATIENT
OUTCOME (n=50)
|
ETIOLOGY |
PATIENT ALIVE n (%) |
PATIENT DIED n (%) |
TOTAL n (%) |
Chi-square χ² |
p VALUE |
OR 95% CI |
|
ISCHEMIC |
12 (70.5%) |
5 (29.5%) |
17 (34%) |
0.025 |
0.873 |
0.90 (0.247
- 3.284) |
|
NON ISCHEMIC |
24 (72.7%) |
9 (27.3%) |
33 (66%) |
|||
|
TOTAL n (%) |
36 (72%) |
14 (28%) |
50 |
Of the total 50 patients:
•
17 (34%) had CAD among which 12 (70.5%) alive & 5 (29.5%)
died.
•
33 (66%) had other etiological factors other than CAD among
which 24 (72.7%) & 9 (27.3%) died.
•
In our study CAD has no significant relationship (p 0.873)
with outcomes.
FIGURE NO 17 : ISCHEMIC VERSUS NON ISCHEMIC

FIGURE NO 18 : CAD VERSUS PATIENT OUTCOME

TABLE NO 11 : SYSTOLIC BP VERSUS
PATIENT OUTCOME (n=50)
|
SYSTOLIC BP (mmhg) |
PATIENT ALIVE n (%) |
PATIENT DIED n (%) |
TOTAL n (%) |
Chi-square χ² |
p VALUE |
OR 95% CI |
|
80-110 |
13 (61.8%) |
8 (38.2%) |
21 (42%) |
1.830 |
0.176 |
0.423 (0.12
- 1.492) |
|
> 110 |
23 (79.3%) |
6 (20.7%) |
29 (58%) |
|||
|
TOTAL n (%) |
36 (72%) |
14 (28%) |
50 |
Of the total 50 patients:
•
21 (42%) had systolic BP between 80-110 mmhg among which 13
(61.8%) alive & 8 (38.2%) died.
•
29 (58%) had systolic BP >110 mmhg among which 23 (79.3%)
& 6 (20.7%) died.
•
In our study systolic BP has no significant relationship (p
0.176) with outcomes.
FIGURE NO 19 : DISTRIBUTION OF PATIENTS BASED ON SYSTOLIC BP

FIGURE NO 20 : SYSTOLIC BP VERSUS PATIENT OUTCOME

TABLE NO 12 : HEART RATE VERSUS
PATIENT OUTCOME (n=50)
|
HEART RATE (bpm) |
PATIENT ALIVE n (%) |
PATIENT DIED n (%) |
TOTAL n (%) |
Chi-square χ² |
p VALUE |
OR 95% CI |
|
≤ 100 |
25 (73.6%) |
9 (26.4%) |
34 (68%) |
0.123 |
0.725 |
1.262 (0.343-
4.647) |
|
> 100 |
11 (68.7%) |
5 (31.3%) |
16 (24%) |
|||
|
TOTAL n (%) |
36 (72%) |
14 (28%) |
50 |
Of the total 50 patients:
•
34 (68%) had HR ≤100 bpm among which 25 (73.6%) alive & 9
(26.4%) died.
•
16 (24%) had HR in between >100 bpm among which 11 (68.7%)
alive & 5 (31.3%) died.
•
In our study heart rate has no significant relationship (p
0.725) with outcomes.
FIGURE NO 21 : DISTRIBUTION OF PATIENTS BASED ON HEART RATE

FIGURE NO 22 : HEART RATE VERSUS PATIENT OUTCOME

TABLE NO 13 : EJECTION FRACTION
VERSUS PATIENT OUTCOME (n=50)
|
EJECTION FRACTION % |
PATIENT ALIVE n (%) |
PATIENT DIED n (%) |
TOTAL n (%) |
Chi-square χ² |
p VALUE |
OR 95% CI |
|
< 50 |
17 (60.7%) |
11 (39.3%) |
28 (56%) |
4.020 |
0.045 |
0.244 (0.058
- 1.024) |
|
≥ 50 |
19 (86.4%) |
3 (13.6%) |
22 (44%) |
|||
|
TOTAL n (%) |
36 (72%) |
14 (28%) |
50 |
Of the total 50 patients:
•
28 (56%) had EF <50% among which 17 (60.7%) alive & 11
(39.3%) died.
•
22 (44%) had EF ≥50% among which 19 (86.4%) alive & 3 (13.6%)
died.
•
In our study ejection fraction has significant relationship (p
0.045) with outcomes.
FIGURE NO 23 : DISTRIBUTION OF PATIENTS BASED ON EJECTION FRACTION

FIGURE NO 24 : EJECTION FRACTION PATIENT OUTCOME

TABLE NO 14 : SERUM SODIUM VERSUS
PATIENT OUTCOME (n=50)
|
SERUM SODIUM meq/L |
PATIENT ALIVE n (%) |
PATIENT DIED n (%) |
TOTAL n (%) |
Chi-square χ² |
p VALUE |
OR 95% CI |
|
≤ 134 |
15 (83.3%) |
3 (16.7%) |
18 (36%) |
1.791 |
0.180 |
2.619 (0.622
- 11.036) |
|
≥ 135 |
21 (65.7%) |
11 (34.3%) |
32 (64%) |
|||
|
TOTAL n (%) |
36 (72%) |
14 (28%) |
50 |
Of the total 50 patients:
•
18 (36%) had serum sodium ≤ 134 meq/L among which 15 (83.3%)
alive & 3 (16.7%) died.
•
32 (64%) had serum sodium ≥ 135 meq/L among which 21 (65.7%)
alive & 11 (34.3%) died.
•
In our study serum sodium has no significant relationship (p
0.180) with outcomes.
FIGURE NO 25 : DISTRIBUTION OF PATIENTS BASED ON SERUM SODIUM

FIGURE NO 26: SERUM SODIUM VERSUS PATIENT OUTCOME

TABLE NO 15 : BLOOD UREA VERSUS
PATIENT OUTCOME (n=50)
|
BLOOD UREA (mg/dl) |
PATIENT ALIVE n (%) |
PATIENT DIED n (%) |
TOTAL n (%) |
Chi-square χ² |
p VALUE |
OR 95% CI |
|
≤ 40 |
19 (90.5%) |
2 (9.5%) |
21 (42%) |
6.130 |
0.013 |
6.705 (1.309-
34.353) |
|
> 40 |
17 (58.7%) |
12 (41.3%) |
29 (58%) |
|||
|
TOTAL n (%) |
36 (72%) |
14 (28%) |
50 |
Of the total 50 patients:
•
21 (42%) had blood urea ≤ 40 mg/dl among which 19 (90.5%)
alive & 2 (9.5%) died.
•
29 (58%) had blood urea > 40 mg/dl among which 17 (58.7%)
alive & 12 (41.3%) died.
•
In our study blood urea has a significant relationship (p
0.013) with outcomes.
FIGURE NO 27 : DISTRIBUTION OF PATIENTS BASED ON BLOOD UREA

FIGURE NO 28 : BLOOD UREA VERSUS PATIENT OUTCOME

TABLE NO 16 : SERUM CREATININE VERSUS
PATIENT OUTCOME (n=50)
|
S.CREATININE (mg/dl) |
PATIENT ALIVE n (%) |
PATIENT DIED n (%) |
TOTAL n (%) |
Chi-square χ² |
p VALUE |
OR 95% CI |
|
≤ 1.3 |
19 (82.7%) |
4 (17.3%) |
23 (46%) |
2.377 |
0.123 |
2.794 (0.738
- 10.58) |
|
> 1.3 |
17 (63%) |
10 (37%) |
27 (54%) |
|||
|
TOTAL n (%) |
36 (72%) |
14 (28%) |
50 |
Of the total 50 patients:
•
23 (46%) had serum creatinine ≤ 1.3 mg/dl among which 19
(82.7%) alive & 4 (17.3%) died.
•
27 (54%) had serum creatinine > 1.3 mg/dl among which 17
(63%) alive & 10 (37%) died.
•
In our study serum creatinine has no significant relationship
(p 0.123) with outcomes.
FIGURE NO 29 : DISTRIBUTION OF PATIENTS BASED ON SERUM CREATININE

FIGURE NO 30 : SERUM CREATININE VERSUS PATIENT OUTCOME

TABLE NO 17 : HEMOGLOBIN VERSUS
PATIENT OUTCOME (n=50)
|
HEMOGLOBIN (gm/dl) |
PATIENT ALIVE n (%) |
PATIENT DIED n (%) |
TOTAL n (%) |
Chi-square χ² |
p VALUE |
OR 95% CI |
|
< 8 |
5 (41.6%) |
7 (58.4%) |
12 (24%) |
7.207 |
0.027 |
6.066 (1.107
- 33.238) |
|
8 - 12 |
18 (81.8%) |
4 (18.2%) |
22 (44%) |
|||
|
> 12 |
13 (81.3%) |
3 (18.7%) |
16 (32%) |
|||
|
TOTAL n (%) |
36 (72%) |
14 (28%) |
50 |
Of the total 50 patients:
•
12 (24%) had Hb < 8 gm/dl among which 5 (41.6%) alive
& 7 (58.4%) died.
•
22 (44%) had Hb in between 8-12 gm/dl among which 18 (81.8%)
alive & 4 (18.2%) died.
•
16 (32%) had Hb > 12 gm/dl among which 13 (81.3%) alive
& 3 (18.7%) died.
•
In our study hemoglobin levels has a significant relationship
(p 0.027) with outcomes.
FIGURE NO 31 : DISTRIBUTION OF PATIENTS BASED ON HEMOGLOBIN LEVELS

FIGURE NO 32 : HEMOGLOBIN VERSUS PATIENT OUTCOME

TABLE NO 18 : SYSTEMIC HYPERTENSION
VERSUS PATIENT OUTCOME (n=50)
|
SHT |
PATIENT ALIVE n (%) |
PATIENT DIED n (%) |
TOTAL n (%) |
Chi-square χ² |
p VALUE |
OR (95% CI) |
|
YES |
11 (61.1%) |
7 (38.9%) |
18 (36%) |
1.654 |
0.198 |
0.44 (0.124
- 1.559) |
|
NO |
25 (78.2%) |
7 (21.8%) |
32 (64%) |
|||
|
TOTAL n (%) |
36 (72%) |
14 (28%) |
50 |
Of the total 50 patients:
•
18 (36%) has HTN among which 11 (61.7%) alive & 7 (38.9%)
died.
•
32 (64%) were normotensive among which 25 (78.2%) alive &
7 (21.8%) died.
•
In our study systemic HTN has no significant relationship (p
0.198) with outcomes.
FIGURE NO 33 : HTN VERSUS NON HTN

FIGURE NO 34 : SYSTEMIC HTN VERSUS PATIENT OUTCOME

TABLE NO 19 : DIABETES MELLITUS
VERSUS PATIENT OUTCOME (n=50)
|
DIABETES MELLITUS |
PATIENT ALIVE n (%) |
PATIENT DIED n (%) |
TOTAL n (%) |
Chi-square χ² |
p VALUE |
OR (95% CI) |
|
YES |
12 (80%) |
3 (20%) |
15 (30%) |
0.680 |
0.409 |
1.833 (0.429
- 7.836) |
|
NO |
24 (68.6%) |
11 (31.4%) |
35 (70%) |
|||
|
TOTAL n (%) |
36 (72%) |
14 (28%) |
50 |
Of the total 50 patients:
•
15 (30%) has DM among which 12 (80%) alive & 3 (20%)
died.
•
35 (70%) were non diabetic among which 24 (68.6%) alive &
11 (31.4%) died.
•
In our study DM has no significant relationship (p 0.409) with
outcomes.
FIGURE NO 35 : DIABETIC VERSUS NON DIABETIC

FIGURE NO 36 : DIABETES VERSUS PATIENT OUTCOME

TABLE NO 20 : DYSLIPIDEMIA VERSUS
PATIENT OUTCOME (n=50)
|
DYSLIPIDEMIA |
PATIENT ALIVE n (%) |
PATIENT DIED n (%) |
TOTAL n (%) |
Chi-square χ² |
p VALUE |
OR (95% CI) |
|
YES |
18 (66.6%) |
9 (33.4%) |
27 (54%) |
0.828 |
0.362 |
0.555 (0.155
- 1.985) |
|
NO |
18 (78.3%) |
5 (21.7%) |
23 (46%) |
|||
|
TOTAL n (%) |
36 (72%) |
14 (28%) |
50 |
Of the total 50 patients:
•
27 (54%) has dyslipidemia among which 18 (66.6%) alive &
9 (33.4%) died.
•
23 (46%) has no dyslipidemia among which 18 (78.3%) alive
& 5 (21.7%) died.
•
In our study dyslipidemia has no significant relationship (p
0.362) with outcomes.
FIGURE NO 37 : DISTRIBUTION OF PATIENTS BASED ON LIPID PROFILE
(DYSLIPIDEMIA)

FIGURE NO 38 : DYSLIPIDEMIA VERSUS PATIENT OUTCOME

TABLE NO 21 : CKD VERSUS PATIENT
OUTCOME (n=50)
|
CKD |
PATIENT ALIVE n (%) |
PATIENT DIED n (%) |
TOTAL n (%) |
Chi-square χ² |
p VALUE |
OR (95% CI) |
|
YES |
7 (58.3%) |
5 (41.7%) |
12 (24%) |
1.462 |
0.226 |
0.434 (0.11
- 1.71) |
|
NO |
29 (76.3%) |
9 (23.7%) |
38 (76%) |
|||
|
TOTAL n (%) |
36 (72%) |
14 (28%) |
50 |
Of the total 50 patients:
•
12 (24%) has CKD among which 7 (58.3%) alive & 5 (41.7%)
died.
•
38 (76%) had either AKI or no renal failure at all among
which 29 (76.3%) alive & 9 (23.7%) died.
•
In our study CKD has no significant relationship (p 0.226)
with outcomes.
FIGURE NO 39 : DISTRIBUTION OF PATIENTS BASED ON RENAL DISEASE (CKD)

FIGURE NO 40 : CKD VERSUS PATIENT OUTCOME

|
STUDY |
PLACE OF STUDY |
n |
TIME PERIOD |
MORTALITY RATE |
PREDICTORS |
|
ADHERE, Adams et al. (15) |
U.S Registry |
33,046 (derivation cohort) 32,229 (validation cohort) |
2001-2003 |
4.2% in-hospital (derivation cohort) 4% in-hospital (validation cohort) |
High blood urea , High serum creatinine |
|
OPTIMIZE-HF |
U.S Registry |
48,612 |
2003-2004 |
3.8% in-hospital mortality |
High serum creatinine , Low serum sodium , Age , Increased heart rate ,
Liver disease , Prior CVA/TIA , PVD , LVSD , COPD |
|
EFFECT, Lee et al. (7) |
Registry |
4,031 |
1997-2001 |
8.9% in-hospital (derivation cohort) 8.2% in-hospital (validation cohort) 10.4%-10.7% at 30 days 30.5%-32.9% at 1 year |
Age , Increased respiratory rate , Hyponatremia , Low hemoglobin , Increased
blood urea , CVA , COPD , Cirrhosis |
|
Sanjay G et al. |
Trivandrum Registry |
1205 |
2013-2017 |
44.8% at 3 years |
Age , NYHA class IV , Increased serum creatinine |
|
Palaniappan M et al. |
Coimbatore |
100 |
2013-2016 |
11% in hospital |
Poor NYHA grade , Presence
of peripheral edema , Low ejection
fraction , High blood urea level , Low hemoglobin level , Presence of chronic
kidney disease |
|
Present Study |
KIMS ,NKP |
50 |
2020-2022 |
28% in hospital |
Age , Prior ADHF , Increased blood urea , Increased serum creatinine ,
Low hemoglobin |
- This is a prospective observational study done over a
period of 2years with a sample size of 50 patients admitted in our
hospital. As discussed earlier, age is an important independent risk
factor for heart failure development61.
- In our study, two thirds of patients are of the age of
41 – 70 years. Less number of patients in above seventy years category may
be explained by a pronounced mortality rate due to disease progression
itself, co-existing non-cardiac diseases and simply aging alone.
- Two thirds of patients were males and it can be partly
explained by life style aspects such as smoking, alcoholism, work stress,
etc that are specific for men at least in India
- In my study 30% has DM , 36% has
HTN , 34% of patients has coronary artery
disease & 54% of patients has dyslipidemia.
·
In our study Age , NYHA class , Ejection fraction , Increased
blood urea , Low hemoglobin levels has significant association with outcomes.
·
The risk stratification model
developed using factors which turned significant in hospital mortality
prediction in large retrospective study on ADHF patients (viz. OPTIMIZE-HF
study) increased age has a higher mortality rate. (OR:1.401 , 95%CI:1.346-1.459
, p value:<0.0001)
·
The acute heart failure study
by EFFECT Lee et al has found a significant relation between increased
age and adverse hospital outcome. (OR:1.83 , 95% CI:1.59-2.10 , p
value:<0.001)
·
In our study age has a significant relationship with
outcomes. (OR:3.391 , 95%CI: 0.655 - 17.556 , p value:0.044).
·
The acute decompensated heart
failure study by Palaniappan M et al has found a significant relation
between poor NYHA class and adverse hospital outcome. (OR:6.000 , 95%
CI:1.242-28.987 , p value:0.014)
·
In our study also NYHA class has significant
relationship with outcomes. (OR:10.00 , 95%
CI: 1.026 -
97.50 , p value:0.044)
·
The risk stratification model
developed using factors which turned significant in hospital mortality
prediction in large retrospective study on ADHF patients (viz. OPTIMIZE-HF
study) indicated that lower ejection fraction (LVSD) on admission would mean a
higher mortality rate.
·
(OR:1.366 , 95%CI:1.226-1.522
, p value:<0.0001)
·
In our study also low ejection fraction (LVSD) has
significant relationship with mortality.
·
(OR:0.244 , 95%CI:0.058 - 1.024 , p value:0.045)
·
Renal failure as evidenced by
elevated urea and impaired creatinine clearance is an important risk factor for
morbidity/mortality of the patients, especially when it worsens rapidly over a
short period of time.
·
The acute heart failure study
by EFFECT Lee et al has found a significant relation between elevated
blood urea and adverse hospital outcome. (OR:1.32 , 95% CI:1.26-1.39
, p value:<0.001)
·
The acute decompensated heart
failure study by Palaniappan M et al has found a significant relation
between high blood urea and adverse hospital outcome. (OR:13.57 , 95%
CI:5.214-35.30 , p value:0.001)
·
In our study also,
elevated blood urea is found to have significant relation with outcomes. (OR:6.705
, 95% CI:1.309-
34.353 , p value:0.013)
·
The acute heart failure study
by EFFECT Lee et al has found a significant relation between low
hemoglobin and adverse hospital outcome. (OR:1.73 , 95% CI:1.25-2.36
, p value:<0.001)
·
The acute decompensated heart
failure study by Palaniappan M et al has found a significant relation
between low hemoglobin and adverse hospital outcome. (OR:14.72 , 95%
CI:1.805-120.67 , p value:0.010)
·
In our study hemoglobin levels has a significant
relationship with outcomes. (OR:6.066 , 95%CI:1.107-33.232
, p value:0.027)
- In my study of all the total 10
patients who recovered completly:
- 8 were alcoholics with wet
beriberi (Thiamine deficiency) who improved drastically with thiamine
supplementation & diuretics.
- They recovered completely and
no recurrence in the follow up as long as they are abstinence from
alcohol.
- 1 patient was with PAH
(Pulmonary Arterial Hypertension) of undetermined etiology
- 1 was the patient with peri
partum cardiomyopathy.
- Mortality rate in my study was
28% with most common cause of death being cardiogenic shock.
·
Following are the limitations to my study:
- Small sample size
- Ideal way to diagnose PAH is by right heart catherization but in our study we are relaying on clinical signs & ECG/2D ECHO findings.
MASTER CHART WITH LINKS TO PATIENTS E-LOG
Link To Master Chart:
PATIENT INFORMATION SHEET
English:
https://drive.google.com/file/d/12LLDgFBVfnTxDdNv5K715uSyLYPUEgrY/view?usp=drivesdk
Telugu:
https://drive.google.com/file/d/13Df9wCu9zhjECpPxcHEULSAphv6-tDHl/view?usp=drivesdk
Template of this "patient information sheet" is borrowed from this website:
https://www.ncbi.nlm.nih.gov/books/NBK261334/
And modified accordingly to my thesis topic.
CONSENT FORMS
REFERENCES:
1.Huffman MD, Prabhakaran D. Heart failure: epidemiology and prevention in India. Natl Med J India. 2010 Sep-Oct; 23(5): 283-8.
2.Felker GM, Leimberger JD, Califf RM, et al. Risk stratification after hospitalization for decompensated heart failure. J Card Fail 2004 Dec;10(6): 460–6.
3.Aronson D, Mittleman MA, Burger AJ. Elevated blood urea nitrogen level as a predictor of mortality in patients admitted for decompensated heart failure. Am J Med 2004 Apr 1;116(7):466 –73.
4.Clinical Quality Improvement Network Investigators. Mortality risk and patterns of practice in 4606 acute care patients with congestive heart failure. The relative importance of age, sex, and medical therapy. Arch Intern Med 1996 Aug 12-26;156(15):1669 –73
5. Fonarow GC, Adams KF Jr, Abraham WT, Yancy CW, Boscardin WJ; ADHERE Scientific Advisory Committee, Study Group, and Investigators. Risk stratification for in-hospital mortality in acutely decompensated heart failure: classification and regression tree analysis. JAMA. 2005 Feb 2;293(5):572-80.
6.Abraham WT, Fonarow GC, Albert NM, et al; OPTIMIZE-HF Investigators and Coordinators. Predictors of in-hospital mortality in patients hospitalized for heart failure: insights from the Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF). J Am Coll Cardiol. 2008 Jul 29;52(5):347-56.
7.Joshi PP, Mohanan CJ, Sengupta SP, Salkar RG. Factors precipitating congestive heart failure--role of patient non-compliance. J Assoc Physicians India. 1999 Mar;47(3):294-5.
8.Bonow RO, Mann DL, Zipes DP, Libby P. Braunwald’s Heart Disease. A textbook of cardiovascular medicine. 9th edition. Page 487 - 502.
9.Fuster, O’Rourke, Walsh, Poole-Wilson. Hurst, The Heart. 12th Edition. Chapter 24. Pathophysiology of heart failure.
10.European Study Group on Diastolic Heart Failure. How to diagnose diastolic heart failure. Eur Heart J. 1998 Jul;19(7):990–1003.




Comments
Post a Comment