Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Symptomatology & event time line:
SOB Grade-II on & off since 20 Years (exacerbations once in a year)
!
Increased frequency & severity of exacerbations since 12 Years
!
T2DM since 8 Years
!
Anemia 5 yrs back treated with iron sucrose
!
Generalized weakness & SOB Grade-II since 30 days
!
HTN since 20 days
!
Pedal edema & Facial puffiness since 15 days
!
SOB Grade-IV & decreased urine output since 2 days
Anatomical localization:
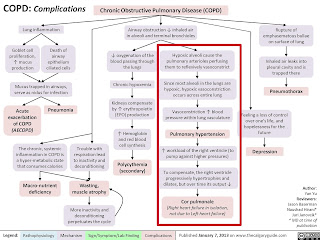
Lungs - COPD - SOB Grade- II
COPD - PAH - RHF - Pedal edema & SOB Grade -IV
Primary etiology:
COPD (Biomass exposure)
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Augmentin:
Azithromycin:
Hydrocortisone:
P - 56 patients hospitalized for AECOPD
I - Group-A : n=29 : Prednisolone
C - Group-B : n=27 : Placebo
O - Follow up at discharge & 6 weeks
At discharge:
Postbronchodilator percentage predicted FEV1 in patients receiving prednisolone had increased significantly in comparison to placebo (47% increase versus 25% increase, respectively; P<0.05).
Until day 5, postbronchodilator FEV1 of the corticosteroid-treated group increased at a significantly accelerated rate compared to placebo (90 mL per day [50.8–129.2] versus 30 mL per day [10.4–49.6], P=0.048).
Patients receiving prednisolone had a significantly shorter median length of hospitalization when compared to placebo (7 days versus 9 days, respectively; P=0.027).
At 6 weeks:
There is no difference in any of these.
CONCLUSION:
Systemic steroids has a role in AECOPD but not in longterm course
Budecort nebulization:
Ipravent: Anticholinergic bronchodilator
Pulmoclear : Acebrophylline + Acetylcysteine
Acebrophylline: Airway mucus regulator with antiinflammatory action.
Acetylcysteine: Reduce the viscosity of sputum facilitating the removal of pulmonary secretions
NON PHARMACOLOGICAL INTERVENTIONS:
1.Head end Elevation:
Significantly increases global and regional end-expiratory lung volume. It has also been shown to improve oxygenation and hemodynamic performance.
2.BiPAP:
By having a custom air pressure for when you inhale and a second custom air pressure when you exhale, the machine is able to provide relief to your overworked lungs and chest wall muscles.
To correct respiratory acidosis
3.Chest physiotherapy:
It is a term used for a group of treatments designed to improve respiratory efficiency, promote expansion of the lungs, strengthen respiratory muscles, and eliminate secretions from the respiratory system.It includes postural drainage, chest percussion, chest vibration, turning, deep breathing exercises, and coughing.
3) What could be the causes for her current acute exacerbation?
It may be due to some bacterial / viral illness / pollutants
4. Could the ATT have affected her symptoms? If so how?
No i don't think so
5.What could be the causes for her electrolyte imbalance?
COPD : the disease process it self may lead to electrolyte imbalance.
HYPONATREMIA in patients with COPD : developed secondary to many reasons, such as development or worsening of hypoxia, hypercapnia, and respiratory acidosis, and right-side heart failure with development of lower limb edema, renal insufficiency, use of diuretics, Syndrome of Inappropriate Antidiuretic Hormone Synthesis, malnutrition, and poor intake during acute exacerbations are common contributing factors in such patients. Activation of the renin-angiotensin-aldosterone system and inappropriately elevated plasma arginine vasopressin in COPD may aggravate the electrolyte imbalance during acute exacerbation of COPD.
HYPOCHLORAEMIA:

2) Neurology (10 Marks)
A) Link to patient details:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Symptomatology & event time line:
Chronic alcoholic since 12 yrs
!
Diabetes since 2 yrs (irregular medications)
!
2-3 episodes of seizures in last 1 year
!
Irrelevant talking , forgetfulness and decreased food intake since 9 days.
Anatomical localization:
Brain : Wernicke's Encephalopathy
Kidney : AKI (pre-renal sec to ?dehydration)
Primary etiology:
Alcohol
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Thiamine: correction of thiamine deficiency
KCL & Potchlor: correction of hypokalemia
Lorazepam: to treat alcohol withdrawl
3) Why have neurological symptoms appeared this time, that were absent during withdrawal earlier? What could be a possible cause for this?
This time he may have developed wernicke's encephalopathy.
Or it may be due to uremic encephalopathy.
Or it may because of kindling in alcohol withdrawl where repeated withdrawls will lead to more severe symptoms.
4) What is the reason for giving thiamine in this patient?
This patient may had thiamine deficiency secondary to chronic alcoholism which is causing wernicke's encephalopathy by various mechanisms.
Thiamine supplementation will lead to improvement of the symptoms and often complete resolution in some cases.
Thiamine administration is usually continued until clinical improvement ceases.
Recovery from the ophthalmoplegia was complete after a few hours, except for a residual, fine, horizontal nystagmus in 60% of patients. Recovery from ataxia occurred after a few days, although in some cases was incomplete. The changes in mental status tended to improve after 2–3 weeks of therapy.
5) What is the probable reason for kidney injury in this patient?
Alcohol - osmotic diuresis - dehydration - pre renal AKI
6). What is the probable cause for the normocytic anemia?
Alcohol abuse and dependence can cause normocytic normochromic anemia through:
- Decreased red blood cell production in the bone marrow - Normocytic normochromic anemia
- Loss of blood through ulcers or inflammation - Iron deficiency anemia which in normocytic normochromic in early stages
- Destruction of red blood cells from heart valve issues, inflammation, immune system damage, or a cancerous tumor - Normocytic normochromic anemia
7) Could chronic alcoholism have aggravated the foot ulcer formation? If yes, how and why?
Chronic alcoholism may lead to foot ulcer formation and delayed healing due to alcoholic neuropathy & malnutrition.
B) Link to patient details:
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Symptomatology & event time line:
Chronic alcoholic & smoker since 30 yrs
!
Giddiness & vomiting 7 days back (relieved with rest)
!
Giddinesss , vomiting , b/l hearing loss , aural fullness , tinnitus , ataxia since 4 days
!
Deviation of mouth & slurring of speech since 1 day
Anatomical localization:
Brain - cerebellar involvement
Primary etiology:
Acute infarct in right inferior cerebellar hemisphere
Risk factors in this patient : Alcohol / Smoking / Denovo HTN
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
VERTIN:
This is betahistine, which is an anti-vertigo medication
MOA- It is a weak agonist on H1 receptors located on blood vessels of the inner ear. This leads to local vasodilation and increased vessel permeability. This can reverse the underlying problem.
Indications- Prescribed for balance disorders. In this case it is used due to patients history of giddiness and balance issues.
ZOFER:
This is ondanseteron- It is an anti-emetic
MOA- It is a 5H3 receptor antagonist on vagal afferents in the gut and they block receptors even in the CTZ and solitary tract nucleus.
Indications- Used to control the episodes of vomiting and nausea in this patient.
ECOSPIRIN
This is aspirin. It is an NSAID (anti-platelet)
MOA- They inhibit COX-1 and COX-2 thus decreasing the prostaglandin level and thromboxane synthesis.
Indications- They are anti platelet medications and in this case used to prevent formation of blood clots in blood vessels and prevent stroke.
CLOPIDOGREL:
It is an antiplatelet medication
MOA- It inhibits ADP mediated platelet aggregation by blocking P2Y12 receptor on the platelets.
Indications- In this case it decreases the risk of heart disease and stroke by preventing clotting.
ATORVASTATIN:
This is a statin group of drug
MOA- It is an HMG CoA reductase inhibitor and thus inhibits the rate limiting step in cholesterol biosynthesis. It decreases blood LDL and VLDL, decreases cholesterol synthesis, thus increasing LDL receptors in liver and increasing LDL uptake and degeneration. Hence plasma LDL level decreases.
Indications- Used to treat primary hyperlipidemias. In this case it is used for primary prevention of stroke.
THIAMINE:
It is vitamin B1
It is naturally found in many foods in the human diet. In this case, the patient consumes excess alcohol- so he may get thiamine deficiency due to poor nutrition and lack of essential vitamins due to impaired ability of the body to absorb these vitamins.
Indications- Given to this patient mainly to prevent Wernickes encephalopathy- that can lead to confusion, ataxia and opthalmoplegia.
3) Did the patients history of denovo HTN contribute to his current condition?
Yes it may be because HTN is an imp risk factor for CVA
4) Does the patients history of alcoholism make him more susceptible to ischaemic or haemorrhagic type of stroke?
Epidemological studies indicate mild to moderate amount of alcohol consumption is protective in ischemic stroke.
Heavy alcohol consumption was associated with increased risk of intracerebral hemorrhage and hemorragic stroke.
Recent heavy alcohol consumption can increase risk for all major types of stroke.
The pathophysiologic mechanisms by which alcohol triggers the onset of spontaneous intracerebral hemorrhage, aneurysmal subarachnoid hemorrhage and ischemic brain infarction remain largely unresolved.
C) Link to patient details:
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Symptomatology & event timeline:
B/l pedal edema since 8 months
!
Dragging type of pain in left UL ass with tingling & numbness
!
Chest pain , palpitations & SOB grade-III since 5 days
Anatomical localization:
Based on the clinical history & limited investigations (ECG not available)
Heart - ? NSTEMI
Primary etiology:
? CAD
2) What are the reasons for recurrence of hypokalemia in her? Important risk factors for her hypokalemia?
Based on the limited data available it is difficult to know the cause of recurrent hypokalemia in this patient.
Further evaluation should be done.
DIAGNOSTIC APPROACH TO HYPOKALEMIA:
3) What are the changes seen in ECG in case of hypokalemia and associated symptoms?
ECG changes:
D) Link to patient details:
QUESTIONS:
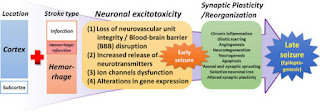
1. Is there any relationship between occurrence of seizure to brain stroke. If yes what is the mechanism behind it?
Going by the history in this patient seizures are secondary to CVA
Mechanism:
2. In the previous episodes of seizures, patient didn't loose his consciousness but in the recent episode he lost his consciousness what might be the reason?
Going by the history previous episodes are focal seizures predominantly involving left side with no LOC (simple partial seizure) and now the recent episode may be a GTCS with LOC
Mechanism of impaired consciousness in seizures:
E) Link to patient details:
Questions:
1) What could have been the reason for this patient to develop ataxia in the past 1 year?
Going by the history in this patient ataxia may be secondary to chronic alcoholism.
ALCOHOL INDUCED CEREBELLAR DEGENERATION
ALCOHOL INDUCED PERIPHERAL NEUROPATHY
2) What was the reason for his IC bleed? Does Alcoholism contribute to bleeding diatheses ?
Most commonly IC bleed is secondary to Trauma or Hypertension.
Going by the history there is no recent fall (trauma).
He is not a known hypertensive either but his ECG is showing features suggestive of LVH (SOKOLOW-LYON CRITERIA : S - wave in V1 + R - wave in V5/V6 > 35 mm)
Which may be secondary to chronic HTN (undiagnosed).
So in this patient based on the data available IC bleed may be secondary to previously undiagnosed HTN.
Or
Heavy alcohol consumption which was associated with increased risk of intracerebral hemorrhage.
Alcohol & bleeding diathesis:
Alcohol (ethanol) intake has effects on platelet aggregation and activation, coagulation factors including von Willebrand factor (vWF), and the fibrinolytic system.
With regard to the effect of alcohol on platelet function, evidence in the literature suggests both platelet activation and platelet inhibition by ethanol. A unifying hypothesis is that platelets are partially activated by ethanol, with partial degranulation allowing for continued circulation of platelets with impaired function. Evidence also exists showing that ethanol intake decreases fibrinogen, factor VII, and vWF levels. In addition, alcohol intake has been found to increase fibrinolysis by increasing tissue plasminogen activator activity.
F) Link to patient details:
Questions
1.Does the patient's history of road traffic accident have any role in his present condition?
No it doesn't
2.What are warning signs of CVA?
3.What is the drug rationale in CVA?
4. Does alcohol has any role in his attack?
Epidemiological evidence indicates that recent heavy alcohol consumption increases the risk for all major types of stroke, whereas light-to-moderate alcohol intake is associated with a decreased risk of ischemic stroke.
The pathophysiologic mechanisms by which alcohol triggers the onset of spontaneous intracerebral hemorrhage, aneurysmal subarachnoid hemorrhage and ischemic brain infarction remain largely unresolved.
The effects of alcohol on hemostasis, fibrinolysis and blood clotting are variable and could either prevent or promote the occurrence of strokes. Regular light-to moderate alcohol consumption seems to afford protection against atherogenesis via several possible mechanisms.
5.Does his lipid profile has any role for his attack??
His lipid profile is with in normal limits - no role in his current problem
G) Link to patient details:
__*Questions*_
1)What is myelopathy hand ?
There is loss of power of adduction and extension of the ulnar two or three fingers and an inability to grip and release rapidly with these fingers.
These changes have been termed "myelopathy hand" and appear to be due to pyramidal tract involvement in various cervical spinal disorders when there is involvement of the spinal cord.
Intrinsic muscle wasting & positive finger escape present.
2)What is finger escape ?
Wartenberg's sign is a neurological sign consisting of involuntary abduction of the fifth (little) finger, caused by unopposed action of the extensor digiti minimi.
This finding of weak finger adduction in cervical myelopathy is also called the "finger escape sign".
3)What is Hoffman’s reflex?
Hoffmann's reflex (Hoffmann's sign, sometimes simply "Hoffmann's", also finger flexor reflex) is involuntary flexion movement of the thumb and or index finger when the examiner flicks the fingernail of the middle finger down. The reflexive pathway causes the thumb to flex and adduct quickly.
A positive Hoffman sign indicates an upper motor neuron lesion and corticospinal pathway dysfunction likely due to cervical cord compression.
However, up to 3% of the population has been found to have a positive Hoffman without cord compression or upper motor neuron disease.
H) Link to patient details:
Possible questions:
1) What can be the cause of her condition ?
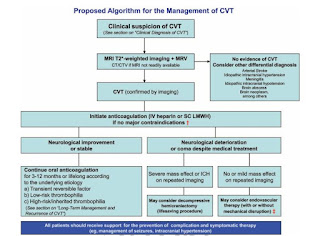
Acute cortical vein thrombosis with hemorrhagic venous infarction involving right posterior temporal lobe.
2) What are the risk factors for cortical vein thrombosis?
3)There was seizure free period in between but again sudden episode of GTCS why?resolved spontaneously why?
Initially patient was completly sedated with midazolam infusion and achieved a seizure free period f/b 1-2 episodes of recurrence after tapering the dose of midazolam which is a common phenomenon.
4) What drug was used in suspicion of cortical venous sinus thrombosis?
Anticoagulants:
Unfractionated heparin / LMWH
3) Cardiology (10 Marks)
A) Link to patient details:
1.What is the difference btw heart failure with preserved ejection fraction and with reduced ejection fraction?
2.Why haven't we done pericardiocentesis in this patient?
This patient had no cardiac tamponade which is an absolute indication for pericardiocentesis.
So we treated him conservatively considering the risks associated with the procedure.
If he had developed cardiac tamponade at any point of time we would have immediately done a pericardiocentesis.
3.What are the risk factors for development of heart failure in the patient?
This patient has most of the risk factors for heart failure like:
- Old age
- T2DM
- HTN
- CAD
- Smoking
- Alcohol
4.What could be the cause for hypotension in this patient?
It may be
B) Link to patient details:
Questions:
1.What are the possible causes for heart failure in this patient?
Old age
T2DM
HTN
Alcohol
CAD
CKD
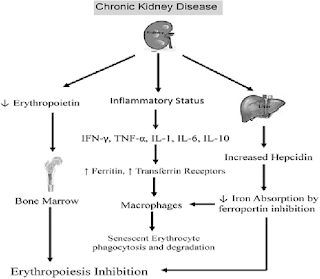
2.what is the reason for anaemia in this case?
Anemia of chronic disease
CKD & ANEMIA:
CHRONIC HEART FAILURE & ANEMIA:
CKD < > HEART FAILURE < > ANEMIA : All these are interlinked with each other.
3.What is the reason for blebs and non healing ulcer in the legs of this patient?
DIABETES
4. What sequence of stages of diabetes has been noted in this patient?
This patient is in stage-IV T2DM with established end stage micro & macro vascular complications.
C) Link to patient details:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Symptomatology & event timeline:
Chronic alcoholic
!
NSAID abuse since 3 yrs
!
Facial Puffiness on & off since 2-3 yrs
!
HTN since 1 year
!
SOB grade : II - IV & decreased urine output since 2 days
!
Anuria since 1 day
!
Denovo DM
Anatomical localization:
Kidney : CKD (?Analgesic Nephropathy)
Heart : HFrEF (?CAD)
Primary etiology:
NSAID abuse
CKD
HTN
T2DM
CAD
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
1. TAB.DYTOR
Mechanism: Through its action in antagonizing the effect of aldosterone, spironolactone inhibits the exchange of sodium for potassium in the distal renal tubule and helps to prevent potassium loss.
2. TAB.ACITROM
Mechanism: Acenocoumarol inhibits the action of an enzyme Vitamin K-epoxide reductase which is required for regeneration and maintaining levels of vitamin K required for blood clotting
3. TAB. CARDIVAS
Mechanism:Carvedilol works by blocking the action of certain natural substances in your body, such as epinephrine, on the heart and blood vessels. This effect lowers your heart rate, blood pressure, and strain on your heart. Carvedilol belongs to a class of drugs known as alpha and beta-blockers.
4. INJ. HAI S/C
Mechanism: Regulates glucose metabolism
Insulin and its analogues lower blood glucose by stimulating peripheral glucose uptake, especially by skeletal muscle and fat, and by inhibiting hepatic glucose production; insulin inhibits lipolysis and proteolysis and enhances protein synthesis; targets include skeletal muscle, liver, and adipose tissue.
5.TAB. DIGOXIN
Meechanism: Digoxin has two principal mechanisms of action which are selectively employed depending on the indication:
Positive Ionotropic: It increases the force of contraction of the heart by reversibly inhibiting the activity of the myocardial Na-K ATPase pump, an enzyme that controls the movement of ions into the heart.
3) What is the pathogenesis of renal involvement due to heart failure (cardio renal syndrome)? Which type of cardio renal syndrome is this patient?
CARDIORENAL SYNDROME - IV
4) What are the risk factors for atherosclerosis in this patient?
Old age
Male gender
Alcohol
HTN
T2DM
CKD
5) Why was the patient asked to get those APTT, INR tests for review?
Patient was kept on T.ACITROM (ACENOCOUMARAL) which is an anti coagulant and was discharged.
So to moniter the response to treatment & maintain it within a therapeutic range, to provide the benefits of anticoagulation, while avoiding the risks of haemorrhage PT , INR & APTT are monitored frequently.
D) Link to patient details:
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Symptomatology & event timeline:
T2DM since 12 yrs
!
On & off chest pain since 1 year
!
TB 7 months back - used ATT for 6 months
!
HTN since 6 months
!
Profuse sweating & SOB grade : III - IV since 30 min
Anatomical localization:
Heart : CAD : NSTEMI
Primary etiology:
T2DM & HTN - CAD
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
TAB MET XL contains Metoprolol as active ingredient
MOA: cardioselective beta blocker
Beta blockers work by blocking the effects of the hormone epinephrine, also known as adrenaline. Beta blockers cause your heart to beat more slowly( negative chronotropic effect)
and with less force( negative inotropic effect). Beta blockers also help open up your veins and arteries to improve blood flow.
Indications: it is used to treat Angina, High blood pressure and to lower the risk of hear attacks.
3) What are the indications and contraindications for PCI?
INDICATIONS:
Acute ST-elevation myocardial infarction (STEMI)Non–ST-elevation acute coronary syndrome (NSTE-ACS)Unstable angina.Stable angina.Anginal equivalent (eg, dyspnea, arrhythmia, or dizziness or syncope)High risk stress test findings. CONTRAINDICATIONS:
Intolerance for oral antiplatelets long-term.Absence of cardiac surgery backup.Hypercoagulable state.High-grade chronic kidney disease.Chronic total occlusion of SVC.An artery with a diameter of <1.5 mm.
4) What happens if a PCI is performed in a patient who does not need it? What are the harms of over treatment and why is research on over testing and over treatment important to current healthcare systems?
Over diagnosis is which occurs when a true abnormality is discovered, but detection of that abnormality and its treatment does not benefit the patient.
Over diagnosis will lead to over treatment , psychological effects & economic burden.
To prevent these adverse events more research is important in this over diagnosis & over treatment.
E) Link to patient details:
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Symptomatology & event timeline:
T2DM & HTN since 8 yrs
!
Chest pain since 3 days
!
Giddiness & profuse sweating since 1 day
Anatomical localization:
Heart : Inferior wall MI
Primary etiology:
Acute inferior wall MI
T2DM , HTN leading to CAD
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
ANTI PLATELETS: ASPIRIN + CLOPIDOGREL
STATINS:
PTCA:
CLINICAL INDICATIONS OF PTCA:
- Acute ST - elevation myocardial infarction ( STEMI )
- Non ST - elevation acute coronary syndrome ( NSTE-ACS )
- Unstable angina
- Stable angina
- Anginal equivalent (eg; dyspnoea, arrhythmia, or dizziness or syncope )
- High risk stress test findings.
3) Did the secondary PTCA do any good to the patient or was it unnecessary?
Secondary PTCA was unnecessary in the patient as he already crossed the window period of 12 hours and was doing fine without PTCA.
F) Link to patient details:
1. How did the patient get relieved from his shortness of breath after i.v fluids administration by rural medical practitioner?
Here the history itself is not clear like what was given and he may have given some diuretic also which decreased his SOB.
Clearly its not the IV FLUIDS which releived his SOB.
2. What is the rationale of using torsemide in this patient?
Torsemide : loop diuretic
This patient is in fluid overload & heart failure where diuretics are the main stay of treatment (reducing preload)
3. Was the rationale for administration of ceftriaxone? Was it prophylactic or for the treatment of UTI?
No its not prophylactic
H/o whitish discharge & TLC was 18000 which clearly indicates infection for which ceftriaxone was given.
4) Gastroenterology (& Pulmonology) 10 Marks
A) Link to patient details:
QUESTIONS:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Symptomatology & event time line:
Chronic alcoholic since 9 yrs
!
Pain abdomen & vomiting 5 yrs back - treated conservatively
!
Stopped alcohol for 3 yrs
!
Again started drinking from last 1 year
!
Recurrent episodes (5-6) of pain abdomen & vomiting in last 1 year
!
Increased alcohol consumption since last 20 days
Last binge 1 week back
!
Pain abdomen & vomiting since 1 week
!
Fever , burning micturition & constipation since 4 days
Course in hospital:
Admitted in hospital and treated conservatively
!
3-4 days later clinical deterioration with SIRS (tachypnea , tachycardia (SVT) , leucocytosis , fever , SOB)
!
Malecot drains were placed for psuedocyst & peripancreatic collections
!
ICD was placed for left sided hydropneumothorax
!
Escalation of antibiotics & other symptomatic treatment continued
!
Clinical improvement with resolution of symptoms and was discharged in a hemodynamically stable state 10 days later
Anatomical localization :
1.Pancreas
2.Lungs
Primary etiology:
ALCOHOL
!
Pancreatitis
!
Pseudocyst & peri pancreatic collections
!
Pancreatico pleural fistula
!
Pleural effusion(exudative)
!
Broncho pleural fistula
!
Hydropneumothorax
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
OCTREOTIDE:
P : 302 patients from 32 hospitals fulfilling the criteria for moderate to severe acute pancreatitis within 96 hours of the onset of symptoms
I : Groups 01 (n=98) and 02 (n=101) received 100 and 200 μg of octreotide, respectively, by subcutaneous injection three times daily for seven days
C : Group P (n=103) received placebo
O : No significant differences among treatment groups with respect to mortality (P: 16%; O1: 15%; O2: 12%), the rate of newly developed complications, the duration of pain, surgical interventions, or the length of the hospital stay.
This trial shows no benefit of octreotide in the treatment of acute pancreatitis.
PANTOP:
P : 40 patients with acute pancreatitis
I : Group - A : Given pantoprazole 40mg BD
C : Group - B : Not given pantop
O : No significant difference in clinical course or outcome
In an experimental study with rats it shows PPZ possesses anti-inflammatory in vivo properties and attenuates the course of AP. This is mediated via a reduced expression of inflammatory and adhesive proteins with a consecutive decrease in platelet and leukocyte activation as key steps in the pathogenesis of AP.
PERCUTANEOUS DRAINAGE:
Early and aggressive intervention helps reduce the morbidity and mortality by preventing the evolution of MODS.
Percutaneous catheter drainage can be a primary treatment option for necrotizing pancreatitis. In addition, it helps to stabilize critically ill patients and delay the surgical procedure to beyond 4 weeks to improve the surgical outcomes.
TPN:
Positively affect the course of the disease and improves the outcome.
FLUID MANAGEMENT:
Fluid therapy has the potential to reduce the progression of pancreatic necrosis and its associated risk of mortality.
Approach to this patient:
Even i would follow the same approach as the treating team and would go for MRCP/ERCP & cystogastrostomy if indicated.
B) Link to patient details:
1) What is causing the patient's dyspnea? How is it related to pancreatitis?
The patient has mild b/l pleural effusion which may be causing his dyspnea.
Two main causes of pleural effusion are:
• Transdiaphragmatic lymphatic blockage leading to increased permiability.
• Pancreaticopleural fistulae secondary to leak and disruption of the pancreatic duct or pseudocyst caused by an episode of acute pancreatitis.
These changes are mediated by inflammatory cytokines.
2) Name possible reasons why the patient has developed a state of hyperglycemia.
3) What is the reason for his elevated LFTs? Is there a specific marker for Alcoholic Fatty Liver disease?
Chronic alcoholism
Specific markers for Alcoholic Liver Disease:
•AST level is more than twice that of ALT
• Elevated levels of Gamma Glutamyl Transferase (GGT)
4) What is the line of treatment in this patient?


C) Link to patient details:
Questions:
1) what is the most probable diagnosis in this patient?
Ruptured liver abscess
Organized collection secondary to hollow viscus perforation.
2) What was the cause of her death?
SEPSIS with MODS
But again etiology can be confirmed only by exploratory laporotomy.
3) Does her NSAID abuse have something to do with her condition? How?
If at all it is a hollow viscus perforation it can be secondary to her NSAID abuse.
NSAID abuse may lead to grade-3 RPD changes in kidney
CKD (?Analgesic Nephropathy)
5) Nephrology (and Urology) 10 Marks
A) Link to patient details:
1. What could be the reason for his SOB ?
Metabolic acidosis
2. Why does he have intermittent episodes of drowsiness ?
Hyponatremia
3. Why did he complaint of fleshy mass like passage in his urine?
It may be the fleshy tissues of prostate post TURP
4. What are the complications of TURP that he may have had?
Hyponatremia
Renal failure
Infection
B) Link to patient details:
Questions
1.Why is the child excessively hyperactive without much of social etiquettes ?
Here in this case the child seems to be psychosomatic , hence the behaviour.
2. Why doesn't the child have the excessive urge of urination at night time ?
Here the child has excessive urge to urinate during day time even though bladder isn’t full because of his psychological impulse to urinate.
During night time as he is asleep he wouldn’t have compulsion to do so.
Psychosomatic overactive bladder
Here the cause of overactive bladder is a condition called pollakiuria, or frequent daytime urination syndrome. Children who have pollakiuria urinate frequently. In some cases, they may urinate every five to 10 minutes or urinate between 10 and 30 times a day. This condition is most common among children aged 3 to 8 and is present only during waking hours. There are no other symptoms present. Doctors believe that pollakiuria is related to stress.
3. How would you want to manage the patient to relieve him of his symptoms?
It is usually unnecessary to treat pollakiuria. The symptoms should subside within a few weeks of starting. In some cases, however, it may take 7-12 months to clear up completely.
It is also helpful to try to identify possible triggers & avoid them.A trigger could be anything that causes the child stress.
Psychological counselling can be done.
6) Infectious Disease (HI virus, Mycobacteria, Gastroenterology, Pulmonology) 10 Marks
A) Link to patient details:
Questions:
1.Which clinical history and physical findings are characteristic of tracheo esophageal fistula?
In this patient perse there are no definitive clinical signs/symptoms characteristic of TEF except for regurgitation & cough on taking foods which may be seen in TEF but not again definitive for TEF.
Here in this case we suspected TEF which is an incidental finding on barium swallow done for dysphagia evaluation.
2) What are the chances of this patient developing immune reconstitution inflammatory syndrome? Can we prevent it?
As this patients latest CD4 count is 91, i think we need to stop ART and start ATT f/b ART initiation 6-8 wks later to prevent IRIS.
7) Infectious disease and Hepatology:
Link to patient details:
1. Do you think drinking locally made alcohol caused liver abscess in this patient due to predisposing factors present in it ?
Amoebic liver abscess (ALA ) seen commonly in the tropics is predominantly confined to adult males, especially those who consume locally brewed alcohol, although intestinal amoebiasis occurs in all age groups and in both genders.
It has been argued that socioeconomic factors and poor sanitary conditions are the primary culprits that casually link alcohol to ALA.
However , there has emerged an abundance of data that implicates alcohol in a more causal role in facilitating the extra-intestinal invasion of the infective protozoan and the subsequent development of ALA.
What could be the cause in this patient ?
## Hence the consumption of locally brewed alcohol is the most likely cause of Liver abscess in this patient.
2. What is the etio-pathogenesis of liver abscess in a chronic alcoholic patient ? ( since 30 years - 1 bottle per day)
PATHOPHYSIOLOGY OF AMOEBIC LIVER ABSCESS
3. Is liver abscess more common in right lobe ?
Yes most common lobe involvement in liver abscess is right lobe.
STREAMLINE EFFECT OF PORTAL CIRCULATION IS CAUSATIVE FACTOR!
( explained below )
This is attributed to the fact that blood from superior mesenteric vein goes preferentially to the right hepatic lobe, while splenic and inferior mesenteric veins divert preferentially to the left lobe.
4.What are the indications for ultrasound guided aspiration of liver abscess ?
INDICATIONS OF LIVER ABSCESS DRAINAGE:
1) If the abscess is large ( 5cm or more ) because it has more chances to rupture.
2) If the abscess is present in left lobe as it may increase
the chances of peritoneal leak & pericardial leak.
3) If the abscess is responding to the drugs for 7 days or more days
METHOD OF ABSCESS DRAINAGE:
Aspiration done using needle or catheter under imaging.
B) Link to patient details:
QUESTIONS:
1) Cause of liver abcess in this patient ?
Considering the following factors:
Age and gender of patient: 21 years (young age) and male.
Single abscess.
Right lobe involvement.
## The abscess is most likely AMOEBIC LIVER ABSCESS
Consumption of locally brewed alcohol or toddy may be the most likely cause of Liver abscess in this patient.
It has been argued that socioeconomic factors and poor sanitary conditions are the primary culprits that casually link alcohol to ALA.
However , there has emerged an abundance of data that implicates alcohol in a more causal role in facilitating the extra-intestinal invasion of the infective protozoan and the subsequent development of ALA.
2) How do you approach this patient ?
3) Why do we treat here ; both amoebic and pyogenic liver abscess?
Considering the following factors:
Age and gender of patient: 21 years (young age) and male.
Single abscess.
Right lobe involvement.
The abscess is most likely AMOEBIC LIVER ABSCESS
But most of the patients with amoebic liver abscess have no bowel symptoms, examination of stool for ova and parasite and antigen testing is insensitive and insensitive and not recommended.
Considering the risk factors associated with aspiration of pus (c/s & microscopy) like:
1) Sometimes abscess is not accessible for aspiration if it is in posterior aspect or so.
2) Sometimes it has thin wall which may rupture if u aspirate.
3) Sometimes it is unliquefied where aspiration is not possible
And due to lack of resources we cant confirm whether it is pyogenic/amoebic , so we treat them both empirically in clinical practice.
4) Is there a way to confirm the definitive diagnosis in this patient?
Yes in a high resource setting definitive cause of liver abscess can be determined using multiple diagnostic strategies, including blood cultures, Entamoeba serology, liver abscess aspirate for culture and molecular and antigen testing.
8) Infectious disease (Mucormycosis, Ophthalmology, Otorhinolaryngology, Neurology) 10 Marks
A) Link to patient details:
Questions :
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Symptomatology & event timeline:
HTN since 2 yrs
!
COVID-19 vaccination 15 days back
!
Fever since 10 days
!
Generalized weakness , facial puffiness & peri orbital edema since 1 week
!
Weakness of right UL & LL since 4 days
!
Altered sensorium since 2 days
!
Denovo T2DM
Anatomical localization:
Oral cavity , nose & orbit : Oro rhino orbital mucormycosis
Brain : CVA (Acute infarct in left frontal & temporal lobes)
Primary etiology:
Diabetes -- mucormycosis
Mucormycosis -- CVA (Acute infarct in left frontal & temporal lobes
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
AMPHOTERICIN-B
3) What are the postulated reasons for a sudden apparent rise in the incidence of mucormycosis in India at this point of time?




































































Comments
Post a Comment