202103254
A 54year old male patient Came to the OPD with chief c/o cough with expectoration since 6 days and low-grade fever since 6 days.
Patient was Apparently asymptomatic 3yrs back then he developed shortness of breath initially grade-2 which progressed to grade 3-4 @ present
B/L pedal oedema since 18 months which is of pitting type.
Bendopnoea & PND since 6months. Palpitations since 6 months.
? episodes of syncopal attacks since 6months.
Orthopnea Since 3months. Nocturia since 2months and insomnia since 2 months and daytime somnolence present.
No H/O chest pain, haemoptysis, vomiting, abdominal pain, Burning micturition no h/o increased frequency, urgency.
History of TB 16 years back for which he was treated.
Not a k/c/o DM/HTN/Asthma/Epilepsy/CAD
Mixed diet, loss of appetite, regular bowel & bladder movements.
Consumption of 180to 360 ML of alcohol daily for the past 10 years.
No known allergies
General examination:
Patient is conscious, coherent, cooperative.
Pallor +, B/L pedal edema +
No signs of icterus, cyanosis, clubbing, generalised lymphadenopathy
Vitals-
Bp: 110/60 mm hg
PR:118 bpm
RR:16cpm
Spo2:82% @ RA - 100% @ 4 lit O2
Temp : afebrile.
Cvs:
Jvp raised
Precordial pulsations +
RV type apex
Epigastric pulsations +
Palpable P2 +
s1 s2 + , no murmers
Respiratory system:
Dyspnea present
Centrally positioned trachea
Reduced chest movement on left side
BAE+ Decreased BS on Left side
NVBS
Crepts heard at B/l Subscapular, inter-scapular, infra scapular areas and infra axillary area
Abdomen:
Soft, non-tender, bowel sounds heard.
CNS:
No abnormality detected.
Provisional diagnosis:
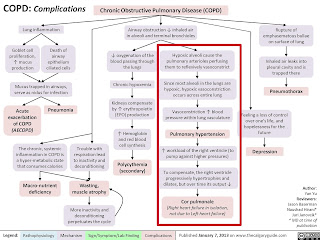
HFmEF secondary to ? Old pulmonary TB (cor pulmonale)
Treatment:
TAB.LASIX 40mg BD
O2 Supplementation @ 4 lit
BP/PR/Temp/ SpO2 monitering 4th hourly















Comments
Post a Comment