BIMONTHLY INTERNAL ASSESSMENT - MARCH 2021
QUESTION 1
Please go through the patient data in the links below and answer the following questions:
https://ashakiran923.blogspot.
a). What is the problem representation of this patient and what is the anatomical localization for his current problem based on the clinical findings?How specific is his dilated superficial Abdominal vein in making diagnosis?
60 year old male chronic smoker & alcoholic non diabetic & non hypertensive
c/o fever since 15 days associated with burning micturition, on & off facial puffiness , abdominal distention , SOB Grade -2 which progressed to Grade -4 , aphthous ulcers & dysphagia.
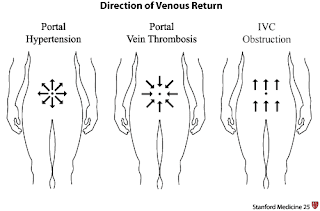
O/E: Distended abdomen with dilated superficial abdominal vein
Shifting dullness +
Localization: Cirrhosis of liver with portal hypertension
UTI
AKI on CKD
b) What is the etiology of the current problem and how would you as a member of the treating team arrive at a diagnosis? What is the cause of his hypoalbuminemia?Why is the SAAG low?
The etiology of the disease in this patient could be a chronic history of alcoholism.
Based on his history & clinical findings : chronic alcoholism ----> cirrhosis of liver ----> portal HTN
Cirrhosis of liver ----> reduced protein synthesis ----> decreased serum albumin ----> hypoalbuminemia.
Hypoalbuminemia can also be due to either increased excretion of protein in urine - nephrotic syndrome (Low SAAG)
Or a long standing infectious etiology causing cachexia and hypoproteinemia (malnutrition / negative acute phase reactant)
Chronic smoking may be the cause of his apthous ulcers.
Low SAAG is because this patient may have exudative pathology.
c)Will PT,INR derangement preceed hypoalbuminemia in liver dysfunction??Share reference articles if any!
The liver plays a central role in the clotting process, and acute and chronic liver diseases are invariably associated with coagulation disorders due to multiple causes: decreased synthesis of clotting and inhibitor factors, decreased clearance of activated factors, quantitative and qualitative platelet defects, hyperfibrinolysis, and accelerated intravascular coagulation.
d)What is the etiology of his fever and pancytopenia?
1) May be bone marrow tuberculosis because ascites is low SAAG ( exudative : ?TB) and same tuberculus bacillus may be invading the bone marrow
2) May be liver dysfunction causing haematological abnormalities like anemia and thrombocytopenia
e)Can there be conditions with severe hypoalbuminemia but no pedal edema? Can one have hereditary analbuminemia and yet have minimal edema? Please go this article https://www.
Inflammation and infection
Albumin is considered a negative acute phase reactant, which means that as inflammation and other acute physiologic processes occur, its levels decrease
In liver disease:Albumin is synthesized in the liver, and low serum albumin can be indicative of liver failure or diseases such as cirrhosis and chronic hepatitis. If present, hypoalbuminemia is generally considered to be a sign of advanced hepatic cirrhosis, or irreversible damage to the liver
Malnutrition or malabsorption
Low albumin levels can also indicate chronic malnutrition from protein losing enteropathy.[3] This is often caused or exacerbated by ulcerative colitis, but can also be seen in cardiac disease and systemic lupus erythematosus.
Conditions with severe hypoalbuminemia and no pedal edema- There can be a compensatory synthesis of protiens (globulins) other than albumin and thereby maintain the oncotic pressure in the intravascular compartment and preventing the extravasation of fluid. This could also be possible if there is a hypovolemic state in the same patient with hypoalbuminemia so that the pressures are again maintained and there is no fluid accumulation.
It is possible for one with hereditary analbuminemia to not have pedal edema. Since it is a chronic and hereditary disease there can be compensatory synthesis of other plasma proteins.
f) What is the efficacy of each of the drugs listed in his current treatment plan
Tamsulosin :
1.α1-Adrenergic receptor antagonists are used by 80% of physicians as the first agent to treat patients with benign prostatic hyperplasia (BPH) presenting with lower urinary tract symptoms (LUTS); 27 of 30 clinical trials have confirmed that α-blockers are effective for BPH treatment.
2.Tamsulosin's α1A subtype adrenergic receptor selectivity is considered to be responsible for its low cardiovascular side effects and lack of interaction with antihypertensives.
3.A 4-year extension, multicenter, open-label, phase IIIB clinical study evaluated long-term efficacy, safety, and tolerability of tamsulosin for up to 6 years; the study found a consistent statistically significant improvement in AUA symptom scores over 6 years, and most patients showed improvement during the first year that was sustained over 6 years.
4.The low incidence of acute urinary retention in patients treated with tamsulosin for up to 6 years suggests that tamsulosin may reduce the risk of AUR in patients with BPH.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1477608/
Nitrofurantoin
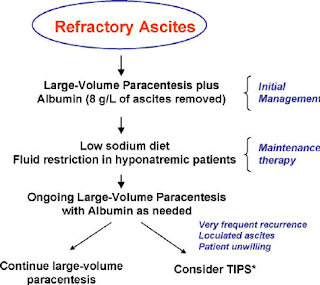
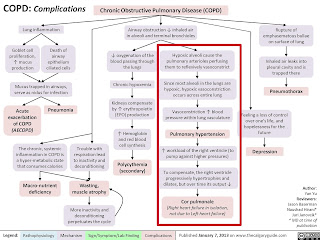
COPD ----> RHF (corpulmonale) ----> Pre renal AKI (?CRS-1) & ?Congestive hepatopathy ----> Ascites
SAAG is 1.9 suggestive of portal hypertensive but low asctic protein of 2.1 and one of the important cause of high SAAG low protein is cirrhosis of liver which can be attributed to alcohol but USG abdomen shows normal liver.
So the other differential is heart failure causing ascites (but ascitic protein should be more than 2.5)
But by going through the events it could be a mixed ascites.
1. LASIX : Mortality: 3 placebo-controlled trials (n=221) reported data; the OR was 0.25 (95% confidence interval, CI: 0.07, 0.84, P=0.03), representing an absolute risk reduction of 8% in mortality in patients treated with diuretics compared to placebo.
Worsening of heart failure: 4 placebo-controlled trials (n=448) and 4 active-controlled trials (n=177) reported data. The OR was 0.31 (95% CI: 0.15, 0.62, P=0.001) for the placebo-controlled trials and 0.34 (95% CI:0.10, 1.21, P=0.10) for the active-controlled trials.
2. SALT AND FLUID RESTRICTION
https://pubmed.ncbi.nlm.nih.gov/23787719/
Individualized salt and fluid restriction can improve signs and symptoms of CHF with no negative effects on thirst, appetite, or QoL in patients with moderate to severe CHF and previous signs of fluid retention.








Comments
Post a Comment