Medical terminologies familiarity including areas of anatomy, physiology, pathology, ML, AI
Empathy and medical humanities
Current EBM strategies for managing diagnostic and therapeutic uncertainty
Section 1) Please go through the patient data in the links below and answer the following questions:
Anatomic and physiologic localization of symptomatology
In patient's own voice:
Patient 1
"I suffered from bad cramps and loose stool movements – and not the usual stomach cramps, it felt like someone was trying to tear out my insides.
On top of that, I was constantly bloated, suffered from bad mouth ulcers, mood swings, hot and cold chills, weight loss, and the dreaded haemorrhoids. It was only in the last year that I started noticing a lot of blood in my stools (lovely I know). My whole body was in pain, from my joints to my muscles, and to my mental state. This led to me becoming quite depressed and anxious, making matters a whole lot worse."
Patient 2:
"I had just gotten back from a holiday with a group of my friends when I had to leave work. I was experiencing constant fever symptoms, I fainted a few times and I was going to the toilet about 15-20 times a day. Not only this but every time I had to use the toilet I was losing blood"
Quoted above from: www.irishtimes.com/life-and-style/health-family/my-daily-routine-living-with-inflammatory-bowel-disease-1.3368509?mode=amp
Patient 3
"2004 and early 2005 were the the darkest days of my life. With no proper diagnosis and treatment, I was going nowhere. Every day was a challenge. I cloud barely drink a glass of fruit juice. No question of taking solid food. Just a bit of solid food in my mouth, it used to cause intense burning. If I managed to forcefully swallow some food, I used to vomit immediately. I was weighing 30kg, just skin and bones. Everyone lost hope, I was not knowing what went wrong and on top of that, everyone who came to see me used to say " your parents and doctors are putting all the efforts to make you healthy, but you don't seem to put any kind of effort or show any intension to get better. Looks like you are enjoying being sick and you want to remain sick.
They were giving me all kinds of suggestions ' why don't you eat, why don't you get up from the bed etc etc. I felt inside ' if these people, even for a minute, go through, the kind of pain I'm bearing for years and, manage to live for a couple of days, I would listen to their suggestion.
Suicidal thoughts were coming, I decided to end my life, luckily my mother came to my rescue and told me ' if you want to die, you should not die alone, I will also end my life along with you ' she said live and fight. That day I promised her, come what way, I'm not going to give up."
Above quoted from: https://medicinedepartment.blogspot.com/2021/04/empathic-narrative-in-inflammatory.html?m=1
In health professional's notes:
Patient 4:
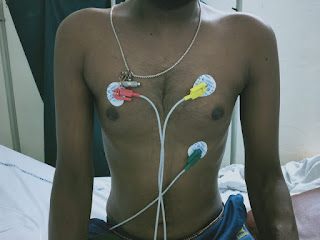
"35/ M who works as a mason presented to us with history of
1) bleeding per rectum -3-4 episodes / day for 2-3 days , associated with hard stools +
Intermittently - for 5-6 months and he Was said to have anal fissure ,used sitz bath and ointment .
No altered bowel habits at that time .
Since December 2020- Patient complaining of - altered bowel habits ,for 10 days he passes stools with normal consistency and frequency then followed by hard stools for 2 days then followed by loose stools -small quantity ,associted with mucus + and blood , foul smelling stools ,2-3 episodes per day ,tenesmus + .no difficulty in flushing stools ,Relieves with fasting .These last for one week , subsides with sitz bath and lignocaine topical application .
Then recurrs again after 10-15 days .
February 2021 - patient had 3 eipsodes of loose stools with severe pain abdomen-left iliac region ,non radiating , he was taken to local hospital ,
Usg - pancreatitis ,Gastritis .
Patient lost 5kgs in 6 months .
No fever ,no joint pains ,no vomitings ,no fresh bleed .
Since 5 days before presenting in April 2021, Patient complaints of loose stools -small quantity , tenesmus + ,with mucus and blood .no pain abdomen"
Question 1) What are the common themes emerging from these symptom narratives? Does the symptomatology related by the patient's own voice evoke more empathy than the one in the health professional notes? Are there studies correlating patient empathy generated in health professionals to disease outcomes or even the doctor patient relationship?
A) * The common theme in all the patient narratives is the agony that they went through and arousing the corner of empathy & giving the closest insight possible…
* Yes definitely ; the symptomatology in patients own voice evoke more empathy than the health professionals notes … since health professional notes is more on the passive note of the patient and it comparatively ( with patient own voice ) lacked the description of all the struggle & suffering of the patient went through!
ROLE OF EMPATHY IN HEALTH PROFESSIONALS AND PATIENT OUTCOMES & DOCTOR— PATIENT RELATIONSHIPS…
* Empathy is the ability to understand and share other people's feelings . It is a core concept as, according to the psychodynamic, behavioral and person-centered approaches, it facilitates the development of a therapeutic relationship with the health care user, providing the basis for therapeutic change
* People with Empathy are welcoming and provide a safe place for people to express their feelings. This ability brings a sense of peace and comfort to others. People with Empathy see the world through the feelings and emotions of others.
* There is a good correlation between physician empathy and patient satisfaction and a direct positive relationship with strengthening patient enablement. Empathy lowers patients' anxiety and distress and delivers significantly better clinical outcomes.
* Empathy as a characteristic of patient–physician communication in both general practice and clinical care is considered to be the backbone of the patient–physician relationship.
* Research has shown empathy and compassion to be associated with better adherence to medications, decreased malpractice cases, fewer mistakes, and increased patient satisfaction!
##These all lead to a good doctor patient relationship…
Question 2) One easily appreciable theme in all these narratives is the impact of the colonic pathology on the patient's psyche with severe symtomatologies precipitating suicidal depression. While the influence of somatic pathology on psyche is easy to appreciate are their studies demonstrating the influence of psyche and life events (that are often part of symptomatology narratives) on disease pathology manifesting in the soma? Please go through the article linked here: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1774724/ and list the evidence for the fact that both chronic stress, in the form of adverse life events, and acute experimental stress can affect systemic immune and inflammatory function, and increase disease activity in humans with IBD.
A) Here ; the patient who was already suffering from inflammatory bowel disease —> had stress and developed psyche —> which inturn exacerbated the already existing pathology of IBD…(may be through psychoneuroimmunology processes)
* Psychological stress has long been reported anecdotally to increase disease activity in inflammatory bowel disease (IBD).
* Recent well designed studies have confirmed that adverse life events, chronic stress, and depression increase the likelihood of relapse in patients with quiescent IBD.
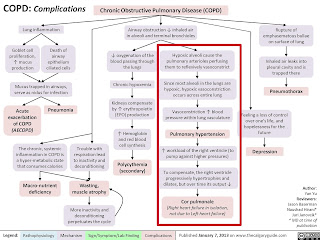
## With the evolving concept of psychoneuroimmunology, the mechanisms by which the nervous system can affect immune function at both systemic and gut mucosal levels are gradually becoming apparent.
* Stress induced alterations in gastrointestinal inflammation may be mediated through changes in hypothalamic-pituitary-adrenal (HPA) axis function and alterations in bacterial-mucosal interactions, and via mucosal mast cells and mediators such as corticotrophin releasing factor (CRF).
Chronic psychological stress, adverse life events, and systemic immune and inflammatory function:
* Chronic sustained stress, such as that due to adverse life events, causes a prolonged increase in cortisol over several days which is characteristically associated with immunosupression.Bereavement, depression, and marital separation have all been shown to reduce the numbers of CD8+ lymphocytes, NK cells, and macrophages found in blood.
Acute psychological stress, experimental stress, and systemic immune and inflammatory function:
* The dichotomous listening test, where different auditory inputs are played into the subject’s ears, has been one of the commonest techniques used to assess the effects of psychological stress on human gastrointestinal physiology.
• Both real life acute stress and experimental stress tests cause acute stimulation of the sympathetic nervous system, with an almost immediate rise in adrenaline and noradrenaline.This is followed by a rise in cortisol but both changes are maintained over only a few hours. Stimulation of the stress axes in this way is associated with immune enhancement.There is an increase in serum levels and the production by whole blood of inflammatory cytokines known to be important in the pathogenesis of IBD

Diagnostic and therapeutic uncertainties
Diagnostic uncertainty:
Patient 3:
"I spent first 10 years of my life absolutely healthy. Started becoming sick after that. Saw few local doctors both allopathy/homeopathy, they said everything was fine, but I wasn't improving. Later met one of the leading gastroenterologist at ABCD Institute of Gastroenterology who diagnosed me as having TB in March 2001 and put on Anti Tuberculosis Treatment for 3 years that ended in march 2004.
After 3 years of pain and suffering, I went from bad to worse. The doctor said ' why did you come again, your treatment is over'. I asked doctor the reason for not recovering he said ' it might not be TB, it might be some other disease, get admitted we will evaluate again'.
I could not digest those words, I was seeing him every fifteen days for 3 years with all the tests and reports.
2004 and early 2005 were the the darkest days of my life. With no proper diagnosis and treatment, I was going nowhere. Every day was a challenge."
Above quoted from:
https://medicinedepartment.blogspot.com/2021/04/empathic-narrative-in-inflammatory.html?m=1
Patient 4:
In this patient logged by our Intern here http://sruthi995.blogspot.com/2021/04/is-online-e-log-book-to-discuss-our.html there was a debate among the health professional team managing him around what if they were missing a tuberculosis of the colon? What if the previous colonoscopy and biopsy had missed the diagnosis of tuberculosis especially as it hadn't been done by a Gastroenterologist but by a general surgeon? While a repeat colonoscopy and biopsy was planned again the expenses were too much to bear for the family members who left after promising to try getting the colonoscopy at a cheaper price from elsewhere and return to us for follow up.
Therapeutic uncertainty:
Patient 1:
"I was taking several different medications at a time for over four months, but the worst of them all was the steroid called prednisone (anyone who has been on these can sympathise with me). These are truly the worst steroids in the world, I gained so much weight, I suffered from moon face, which made me look like a chipmunk (and not a cute one). I started receiving Infliximab (Remicade) infusions every two months, which is an auto-immune suppressant drug used to treat IBD."
Patient 2:
"I thought I could get it under control quickly and everything would go back to the way it was. I was wrong. The first six months after diagnosis were hell on earth. I developed severe anxiety about leaving the house as a result of my illness and symptoms. I tried to return to work and then became depressed when I failed miserably. My relationship ended. I had no appetite and couldn’t put back on the weight which resulted in me feeling really badly about my body and appearance.
I was taking steroids called Prednisone for the first three months and they made my face swell up, my hair fall out and also added massively to the anxiety and depression I was already dealing with. I began getting Infliximab (Remicade) infusions to suppress my immune system every eight weeks. That eventually had to be changed to every six weeks because my symptoms were still quite severe and the medication wasn’t lasting long enough.
Fourteen months down the line after diagnosis I am still struggling. "
Question 3) What are the current computational advances to resolve diagnostic uncertainty for health professionals such as the one described in patient 4? Go through this article: https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-020-01277-w and list the differences in the endoscopy findings between ulcerative colitis and intestinal tuberculosis identified by the Random forest and CNN model. Go through the colonoscopic descriptions captured in the patient 4 online EMR linked above and share your insights on what could be the probable diagnosis. Please share your current general knowledge thoughts or similar past experiences in diagnostic uncertainty while dealing with patients with potential inflammatory bowel disease and how you resolved them.
A) *
The current computational advances in the diagnosis of intestinal tuberculosis include:
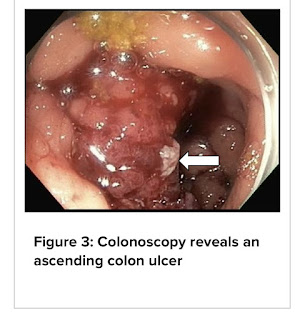
1) COLONOSCOPY:
* Colonoscopy may detect asymptomatic cases when performed for other reasons.Biopsies obtained by colonoscopy have been reported to have as high as 80% diagnostic accuracy. The yield from culture has been reported to be higher when multiple tissue biopsies are obtained during colonoscopy.
* TB of the colon predominantly affects the cecum and the ascending colon. Ulceration, nodularity, and stricture are the prominent endoscopic findings.
TB COLITIS
PATULOUS ILEOCEACAL VALVE WITH ULCERATIVE TUBERCULOSIS
* The availability of colonoscopic biopsy has significantly reduced the need for surgical/laparoscopic access for tissue. Histology is often not definitive for a diagnosis of TB, and culture remains the gold standard.
* Initial diagnosis of “confirmed colon TB” was made if the biopsy specimen showed caseating granulomas and/or acid-fast bacilli.
ILEOCEACAL VALVE BIOPSY SHOWING EXTESNSIVE GRANULOMTOUS INFLAMMATION WITH ACID FAST BACILLI ( top: 10x hematoxylin and eosin stain & bottom: 60x , acid fast stain ) consistent with mycobacterial infection
2) CT SCAN:
* CT scan is the modality of choice in evaluating the extent and type of GI TB. It appears as asymmetric wall thickening of the terminal ileum, cecum, or ileocecal valves associated with necrotic lymph nodes. After chronic inflammation, the cecum may appear small and irregular due to fibrosis and stenosis.
3) OTHERS:
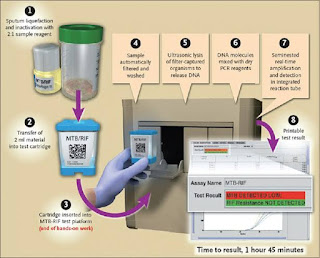
* The Xpert MTB/RIF (rifampicin) assay is a fully automated real-time PCR-based test designed for rapid and simultaneous detection of M. tuberculosis and mutations associated with rifampicin resistance, and the result is available within 2 h .The test is expensive but it is marketed as a point-of-care test and requires virtually no training or laboratory infrastructure.
* A positive GeneXpert-Mtb/Rif helps in the diagnosis of ITB, but the sensitivity is low.
Gene Xpert technique
Below is the algorithm of how to approach a patient suspected of having abdominal tuberculosis:
### Clearly from the above algorithm; it is important to do endoscopy in patients suspected with intestinal tuberculosis…
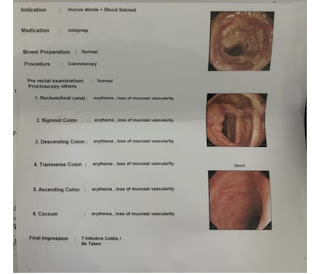
DIFFERENCE IN ENDOSCOPY BETWEEN ULCERATIVE COLITIS AND INTESTINAL TUBERCULOSIS:
* Artificial intelligence through machine learning is very promising in helping unexperienced endoscopists differentiate inflammatory intestinal diseases.
* Below are the colonoscopy findings in the patient no: 4
My insight of this patient is ; he may be having infective colitis…?
Confirmed after the biopsy…. (Question 4)
List the current therapeutic strategies for IBD and share your critical appraisal of a few RCTs around each option, not only those mentioned in the patient narratives above such as SAIDs like prednisolone and biologicals like infliximab but also NSAIDs such as meselamine and immunomodulators such as azathioprine.
Advocacy and pluralistic integration of available solutions as a therapeutic tool.
TREATMENT:
* The goal of inflammatory bowel disease treatment is to reduce the inflammation that triggers your signs and symptoms. In the best cases, this may lead not only to symptom relief but also to long-term remission and reduced risks of complications. IBD treatment usually involves either drug therapy or surgery.
MEDICAL MANAGEMENT:

1) Anti-inflammatory drugs:-
Anti-inflammatory drugs are often the first step in the treatment of inflammatory bowel disease. Anti-inflammatories include corticosteroids ( prednisolone) and aminosalicylates, such as mesalamine (Asacol HD, Delzicol, others), balsalazide (Colazal) and olsalazine (Dipentum). Which medication you take depends on the area of your colon that's affected.
2) Immune system suppressors:-
* These drugs work in a variety of ways to suppress the immune response that releases inflammation-inducing chemicals into the body. When released, these chemicals can damage the lining of the digestive tract.
Some examples of immunosuppressant drugs include azathioprine (Azasan, Imuran), mercaptopurine (Purinethol, Purixan) and methotrexate (Trexall).
3) Biologics:-
* Biologics are a newer category of therapy in which therapy is directed toward neutralizing proteins in the body that are causing inflammation. Some are administered via intravenous (IV) infusions and others are injections you give yourself. Examples include infliximab (Remicade), adalimumab (Humira), golimumab (Simponi), certolizumab (Cimzia), vedolizumab (Entyvio) and ustekinumab (Stelara).
3) Antibiotics:-
* Antibiotics may be used in addition to other medications or when infection is a concern — in cases of perianal Crohn's disease, for example. Frequently prescribed antibiotics include ciprofloxacin (Cipro) and metronidazole (Flagyl).
***Other medications and supplements:-
In addition to controlling inflammation, some medications may help relieve your signs and symptoms, but always talk to your doctor before taking any over-the-counter medications. Depending on the severity of your IBD, your doctor may recommend one or more of the following:
- Anti-diarrheal medications. A fiber supplement — such as psyllium powder (Metamucil) or methylcellulose (Citrucel) — can help relieve mild to moderate diarrhea by adding bulk to your stool. For more-severe diarrhea, loperamide (Imodium A-D) may be effective.
- Pain relievers. For mild pain, your doctor may recommend acetaminophen (Tylenol, others). However, ibuprofen (Advil, Motrin IB, others), naproxen sodium (Aleve) and diclofenac sodium likely will make your symptoms worse and can make your disease worse as well.
- Vitamins and supplements. If you're not absorbing enough nutrients, your doctor may recommend vitamins and nutritional supplements.
Nutritional support:
When weight loss is severe, your doctor may recommend a special diet given via a feeding tube (enteral nutrition) or nutrients injected into a vein (parenteral nutrition) to treat your IBD. This can improve your overall nutrition and allow the bowel to rest. Bowel rest can reduce inflammation in the short term.
If you have a stenosis or stricture in the bowel, your doctor may recommend a low-residue diet. This will help to minimize the chance that undigested food will get stuck in the narrowed part of the bowel and lead to a blockage.
SURGICAL MANAGEMENT:
ULCERATIVE COLITIS AND CHRON’S DISEASE RESPECTIVELY
If diet and lifestyle changes, drug therapy, or other treatments don't relieve your IBD signs and symptoms, your doctor may recommend surgery.
# Sugery for ulcerative colitis : Surgery involves removal of the entire colon and rectum and the production of an internal pouch attached to the anus that allows bowel movements without a bag.
In some cases a pouch is not possible. Instead, surgeons create a permanent opening in your abdomen (ileal stoma) through which stool is passed for collection in an attached bag.
## Surgery for Crohn's disease: Up to two-thirds of people with Crohn's disease will require at least one surgery in their lifetime. However, surgery does not cure Crohn's disease.
During surgery, your surgeon removes a damaged portion of your digestive tract and then reconnects the healthy sections. Surgery may also be used to close fistulas and drain abscesses.
The benefits of surgery for Crohn's disease are usually temporary. The disease often recurs, frequently near the reconnected tissue. The best approach is to follow surgery with medication to minimize the risk of recurrence.

FEW RCT’s ( showing efficacy )
"I tried Allopathy, Ayurveda, Naturopathy, etc. They helped me to some extent, they helped to be alive, but not helped me to the extent I wanted. Then I thought let me try YOGA."
Quoted from here:
Patient 5:
"
You see, it’s really difficult to live with Crohn’s or ulcerative colitis as it is but in many cultures around the world, there is little to no acceptance of young people who have chronic illnesses. And even though I live in cosmopolitan New York City, I have had one foot in two cultures: the country of my origin, India, and the country of my birth, the United States. According to South Asian culture, I was supposed to be taking care of my widowed mother, not being a burden on her. I was supposed to be out working my Wall Street job and supporting my family, not being a frequent flyer on the IBD floor of my hospital. As the oldest child of the family with no father and no brothers, my role was to take care of my family, not be the person being constantly taken care of."
Quoted from here :
Question 5) What is the role of the internet and it's patient users toward driving their own healthcare outcomes through timely sharing of their problems and pluralistic solution inputs from patient advocates and health professionals? What is the role of a doctor patient relationship in healing outcomes as demonstrated in some of the narratives? Please share your own experiences where you were part of one such relationship that worked positively or negatively for your patient. What is the role of computational ML AI in considerably expanding this "user driven healthcare" space? Please search for clinical decision support projects that begin with "applications that assign SNOMED CT codes to entered patient data which in turn trigger decision support information."
Check out how these can be further expanded using ML AI techniques to create knowledge graphs toward
"1) Named-Entity Recognition — given a patient’s initial complaint, the NER should tag medical and clinical entities.
2) Classification — e.g. classify an initial patient chat as an informational session or requires a visit to a hospital.
3) Diagnosis — ability to provide a diagnosis (with certain probability) given a chat session
A) THE IMPACT OF HEALTH INFORMATION TECHNOLOGY ( HIT ) ON PATIENT SAFETY:
* Health information technology improves patient’s safety by reducing medication errors, reducing adverse drug reactions, and improving compliance to practice guidelines
* Healthcare organizations need to be selective in which technology to invest in, as literature shows that some technologies have limited evidence in improving patient safety outcomes.
* Patient safety is a subset of healthcare and is defined as the avoidance, prevention, and amelioration of adverse outcomes or injuries stemming from the processes of health care.
* Healthcare information technology (HIT) has been defined as “the application of information processing involving both computer hardware and software that deals with the storage, retrieval, sharing, and use of health care information, data, and knowledge for communication and decision making”.
* Health information technology includes various technologies that span from simple charting, to more advanced decision support and integration with medical technology.
Some of the various aspects of the HIT in healthcare:
Electronic Medical Record (EMR), Electronic Physician’s Order entry (CPOE), Clinical Decision Support (CDS), E-prescribing, Electronic Sign-out and Hand-off, Bar Code Medication Administration (BCMA), Closed Loop Medication Administration, Patient Data Management Systems (PDMS), Retained Surgical Items Detectors, Patient Electronic Portals, Telemedicine, Electronic Incident Reporting, Intelligent Infusion Devices, Smart Pump, Programmable Pump, Automated Medication Dispensing
Overall impact of EMR on patient safety:
* Numerous studies have considered the outcomes of implementing an electronic medical record on healthcare quality and patient safety, with a majority of studies showing favorable results. Although, some studies demonstrated negative outcomes which continues to evoke dispute.
* Computerized physician order entry and CDS are probably one of the most beneficial health information technologies for improving patient safety.
ROLE OF DOCTOR-PATIENT RELATIONSHIP (DPR) IN HEALING OUTCOMES:
* Effective physician-patient communication has been shown to positively influence health outcomes by increasing patient satisfaction, leading to greater patient understanding of health problems and treatments available, contributing to better adherence to treatment plans, and providing support and reassurance to patients.
* Active listening, responding appropriately to patient's needs and concerns, properly assessing body language, and possessing a non-judgmental attitude are all necessary skills that healthcare workers need to possess.
* Trust in doctors allows patients to effectively discuss their health issues. Development of trust enables the patient to comply with the doctor's guidance, which consequently results in improvement of health.
What are the Benefits of Effective Communication in Healthcare?
- Improved Patient-Provider Interactions. Improved health communication skills between patients and healthcare providers lead to better health outcomes for patients. ...
- Improved Patient Satisfaction. ...
- Decrease Patient Complaints & Readmissions. ...
- Improve Internal Teamwork & Collaboration.
ONE OF MY PERSONAL EXPERIENCE ON DPR AND PATIENT
ROLE OF AI AND ML IN HEALTHCARE :
* Artificial intelligence and machine learning in healthcare will continue to get better and impact disease prevention and diagnosis, extract more meaning from data across various clinical trials, help develop customised drugs based on an individual's unique DNA and inform treatment options among other things.
The future is here!
ARTIFICIAL INTELLIGENCE IN HEALTHCARE SYSTEM:
USAGE OF AI ASSISTED ROBOTICS IN HEALTHCARE
- Utilisation of technology to its high end in healthcare
OVERALL KEY BENEFITS OF AI
MACHINE LEARNING IN HEALTHCARE SYSTEM:
* Full literature ( on ML and AL in healthcare) here :
CLINICAL DECISION SUPPORT PROJECTS:
* A clinical decision support system (CDSS) is a health information technology, provides clinicians, staff, patients, or other individuals with knowledge and person-specific information, intelligently filtered or presented at appropriate times, to enhance health and health care. CDS encompasses a variety of tools to enhance decision-making in the clinical workflow.
##These tools include computerized alerts and reminders to care providers and patients; clinical guidelines; condition-specific order sets; focused patient data reports and summaries; documentation templates; diagnostic support, and contextually relevant reference information, among other tools.
* A working definition has been proposed by Robert Hayward of the Centre for Health Evidence: "Clinical decision support systems link health observations with health knowledge to influence health choices by clinicians for improved health care".
*** CDSSs constitute a major topic in artificial intelligence in medicine.
So now the question is how can it (CDS) be helpful…?
KNOWLEDGE GRAPHS TOWARDS NER, CLASSIFICATION, DIAGNOSIS CREATED USING ML AI TECHNIQUES:
* Some examples include;
Some of the examples chatbots at the user (patient) disposal in healthcare:
(used predominantly for the diagnosis, treatment, constant monitoring, remainding follow ups of the patient)
*chatbots works based on ARTIFICIAL INTELLIGENCE…
*Below is the link for ; Sensely virtual health assistant ‘MOLLY’
Examples of the knowledge graphs in clinical management:
Full literature on how knowledge graphs are made in healthcare using ML and AI ; here:
Finally to sign out on a note around the disease theme in this question paper, from your own user perspective, please critically appraise this paper that develops an "ontology encapsulating IBD physicians knowledge
and describes different characteristics such as classification, medi-
cation, the activity of the disease, diagnosis techniques and various
other IBD attributes along with generating a knowledge graph by
importing 560 patient records collected in their University Hospital ontology."
A) DISEASE THEME OF THIS PAPER IS IBD:
* The theme decided for this year's World IBD Day is "Break the silence".
* This day aims at uniting people and fighting against ulcerative colitis and Crohn's diseasethrough spreading awareness.
## World Inflammatory Bowel Disease (IBD) Day is celebrated every year on May 19th, to raise awareness and improve the lives of people suffering from Crohn’s disease and ulcerative colitis - a type of inflammatory bowel disease.
MY CRITICAL APPRAISAL ON THIS PAPER:
* Firstly ; it gave me insight to the deep struggle & suffering of the patients having IBD by reading all those patient narratives…
— We as health professionals ; just ask for a symptoms ,whether they are present or not.. BUT NEVER BOTHERED ABOUT THE AGONY BURRIED UNDER THOSE SYMPTOMS !
— These patient narratives, definitely aroused a empathetic corner in me…
* Then; I learnt how can a patients misery be with the chronic steroid use ( which a good doctor doesn’t do…)
* I learnt how important a empathy can be in a doctor patient relationship …
* Pathogenic mechanisms and different diagnostic procedures , therapeutic management in the IBD & difference between the UC , CD , ITB ( has minor differences so much that lead to confusion clinically )
* Now coming to the most interesting futuristic topic of the paper :
1) HEALTH INFORMATION TECHNOLOGY (HIT) ON PATIENT SAFETY
2) ROLE OF ML , AI IN HEALTHCARE
• for detection of ailments, treatment, decision making, giving patient superior experience ,etc
• usage of robotics in future medicine practice…
• for drug discovery & manufacturing , medical imaging, smart health records, disease predictions,etc
## CDSS PROJECTS and their benefits…
## Chabots of different entities; interesting how they work…
## knowledge graphs of many aspects in healthcare created by AI and ML process …
* I would like to conclude this discussion by saying that this assignment paper was different than rest of others ; which definitely increases interest and keeps our intriguing minds engaged.I liked doing this assignment and looking forward to do many in this new pattern…































































Comments
Post a Comment