202102692
55 year old farmer came to the casualty with C/O of-
-SOB grade IV since 4days
-Abdominal distention with scrotal swelling since 1week
-SOB on lying down since 3days with pedal edema
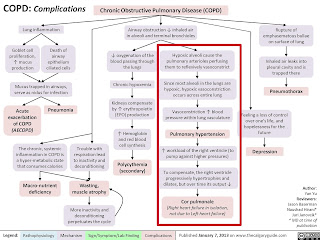
Patient was apparently alright 6years back then developed SOB on doing routine work, progressing to even on walking for short distance, diagnosed as Right Heart Failure on treatment.
Abdominal distention along with pedal edema since 1year, therapeutic tap was done in view of ascites twice before, last done 3months back. Symptoms aggravated since 1week associated with constipation, relieved on taking medication, associated with increasing SOB and Orthopnea.
Associated with decreased urine output intermittently , facial puffiness and anasarca relieved on medication.
Symptoms increased on intake of alcohol, non adherence to diet.
PAST HISTORY-
K/C/O COPD secondary to chronic smoker stopped 4years back gradually over a period of 2 years. 1pack beedi/day for 30years.
K/C/O chronic occasional consumption of whisky. Daily consumption of toddy.
GENERAL EXAMINATION-
Patient is concious, coherent and cooperative.
Patient looks malnourished.
B/L pedal edema present.
No signs of pallor, icterus, cyanosis, lymphadenopathy.
VITALS-
Afebrile
PR-84bpm RR-22cpm
BP-130/70mmhg SpO2-99% at RA
GRBS-148mg/dl
SYSTEMIC EXAMINATION-
CVS- S1 S2 present, Thrills present on left and right parasternal area, visible pulsations. Pansystolic murmur in mitral and tricuspid area.
RS-Dyspnea grade IV, No wheeze, Centrally placed trachea, breath sounds vesicular, no adventitious sounds.
PA-Distented abdomen with fluid:Gross ascites, no tenderness and palpable mass, normal hernial orifice, bowel sounds present.
Genitals- scrotal swelling present.
CNS- Concious with normal speech , no signs of meningeal irritation, no motor, sensory and cranial nerve deficits.GCS-15/15.
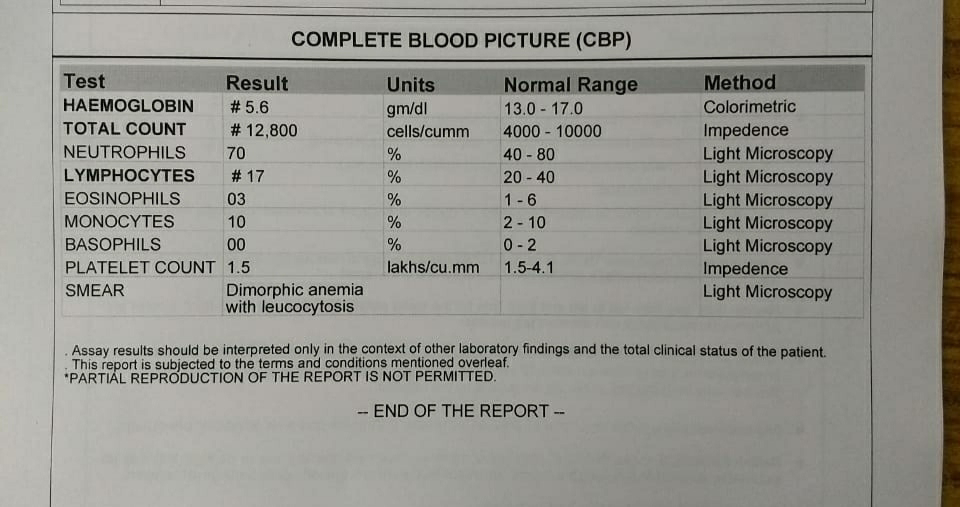
INVESTIGATIONS:
PROVISIONAL DIAGNOSIS- K/C/O COR PULMONALE WITH SEVERE PAH GRADEIII WITH AKI WITH CONGESTIVE HEPATOPATHY WITH GROSS ASCITES WITH ANEMIA UNDER EVALUATION.
TREATMENT
On day of admission-02/02/2021
At 6:00pm RS- BAE present, wheeze present.
SpO2-84% on RA.
91% on 8L oxygen.
1. Propped up position.
2. Fluid restriction to <1.5L/day.
3. Salt restirction to <2gm/day.
4. Inj.LASIX 40mg IV TID if SBP >100mmhg.
5. Oxygenation if spO2<90% RA.
6. DAILY WEIGHT AND ABDOMINAL GIRTH MONITORING.
7.Strict I/O charting.
8. Condom cheterisation.
9. Nebulisation with SALBUTAMOL 2respules 8th hrly and BUDECORT 2respules 12th hrly.
10. Inj. HYDROCORTISONE 100mg IV OD.
11. Inj. VIT K 10mg IV OD.
12. Syp. LACTULOSE 15ml PO BD.
13. Inj. MONOCEF 1gm IV BD.
14. Ascitic tap done and drained 450ml of ascitic fluid.
15. Inj.PANTOP 40mg IV OD.
ON DAY 1-03/02/2021
S-
C/o burning or squeezing pain in the chest, epigastrium. SOB comparatively decreased.
O-
Patient is c/c/c.
Afebrile
BP-140/90mmhg
PR-106bpm
SpO2-85% on 8L oxygen
CVS- JVP increased upto angle of mandible. Visible pulsations on right and left second parasternal spaces. Apical impulse is diffuse, 6th ICS, anterior axillary line. S1 S2 present and muffled in all areas. Pansysyolic murmur ( mitral area>tricuspid area), radiation. Thrill palpable in right parasternal area.
PA- Distended abdomen, flat umbilicus, fluid thrill is absent, shifting dullness is present, soft, non tender. Bowel sounds present.
RS- BAE present, B/L end expiratory wheeze in all areas.
CNS-NAD
A-
K/C/O COR PULMONALE WITH SEVERE PAH GRADEIII WITH AKI WITH CONGESTIVE HEPATOMEGALY WITH GROSS ASCITES WITH ANEMIA UNDER EVALUATION AND THROMBOCYTOPENIA.
P-
TREATMENT
1. Propped up position.
2. Fluid restriction to <1.5L/day.
3. Salt restirction to <2gm/day.
4. Inj.LASIX 40mg IV TID if SBP >110mmhg.
5. Inj. PANTOP 40mg IV OD.
6. Inj. VIT B12 1000mcg IM OD.
7. Inj. VIT K 10mg IV OD.
8. Syp. LACTULOSE 15ml PO BD.
9. Inj. MONOCEF 1gm IV BD.
10. Ascitic tap done and drained 750ml of ascitic fluid.





























Comments
Post a Comment