CHIEF COMPLAINT:
A 42 year old male patient was brought to casuality with chief complaints of bilateral lower limb swelling (pitting type) (l>r) since 15 days, Fever since 7 days and SOB since 2 days.
HISTORY OF PRESENT ILLNESS:
•Patient
was apparently asymptomatic 15 days
back & then he noticed bilateral lower limb swelling which was insidious in
onset gradually progressing pitting type
( left more than right ) extending up to
the knees.
•Patient
had history of trauma over the left malleoli 10 days back followed by an ulcer
& increased swelling of the left
lower limb
•History
of Fever which is low Grade intermittent associated with generalized weakness since 7 days
•Patient
also complaining of breathlessness since 2 days which is Grade 2 initially progressed to Grade 3-4 associated with orthopnea & PND
No h/o cough, chest pain
No h/o pain abdomen, vomiting, loose stools
No h/o decreased urine output/ burning micturition and no other complaints
HISTORY OF PAST ILLNESS:
•In
2018
He
accidentally got injured by an iron rod on left foot big toe which formed into
an ulcer for which he took some symptomatic Rx but it didn’t
subside and the very next day the foot got swollen (?cellulitis) and he
came to our hospital for which he was treated
with antibiotics and other supportive
care f/b SSG to left foot ulcer.
•In
2020
He
had history of fever, decreased appetite, cough for which he went to a local
hospital where he was diagnosed with Tuberculosis and is on irregular
medication
He
was not k/c/o DM , HTN , Bronchial Asthma , Epilepsy CVA CAD
PERSONAL HISTORY:
Diet
– Mixed
Appetite
– Decreased
Sleep
– Decreased
Bladder
& Bowel movements – Regular
He has been consuming alcohol 180ml daily , Chronic
smoker 2 pack beedi/day and khaini 2-3 per day for the past 20 years.
GENERAL EXAMINATION
Patient is conscious,coherent,cooperative
Thin built & moderately nourished
Icterus is present
Pedal edema is present
No pallor, cyanosis, clubbing, lymphadenopathy
VITALS:
1.Temperature:- 98.6 F
2.Pulse rate: 110 beats per min , regular
3.Respiratory rate: 18 cycles per min
4.BP: 100/70 mm Hg
SYSTEMIC EXAMINATION:
A.CARDIOVASCULAR SYSTEM
Inspection:
•Chest
is barrel shaped, bilaterally symmetrical.
•Trachea
is central
•Movements
are equal bilaterally
•JVP:Raised
•Visible
epigastric pulsations
•No
scars or sinuses
•Apical
impulse seen in left 6th intercostal space lateral
to midclavicular line
VISIBLE APEX BEAT
VISIBLE EPIGASRTIC PULSATIONS
Palpation:
•All inspectory findings are confirmed:
Trachea is central, movements equal bilaterally.
•Antero-posterior diameter of chest >Transverse
diameter of chest
•Apex beat felt in left 6th intercostal space lateral
to midclavicular line
•Parasternal heave present (Grade-3)
•Palpable P2 +
Auscultation:
•S1 S2 heard
•No murmurs
RESPIRATORY SYSTEM:
Inspection:
•Chest is barrel shaped, bilaterally symmetrical.
•Trachea is central
•Movements are equal bilaterally
•Visible epigastric pulsations
•No scars or sinuses
•Apical impulse seen in left 6th ICS lateral to MCL
BARREL SHAPED CHEST
Palpation:
•All inspectory findings are confirmed:
Trachea is central, movements equal
bilaterally.
•Antero-posterior diameter of chest
>Transverse diameter of chest
•Apex beat felt in 6th intercostal space
lateral to midclavicular line
•Vocal fremitus decreased in right IAA
& ISA
AP diameter-23cms, Transverse diameter- 23cms
Percussion:
•Dull note heard in right IAA & ISA
•Resonant note heard in all other areas
bilaterally
Auscultation:
•Bilateral air entry present – Normal
vesicular breath sounds heard
•Breath sounds decreased in right IAA &
ISA
•Vocal resonance decreased in right IAA &
ISA
•Expiratory wheeze heard bilaterally
PER ABDOMEN:
•Scaphoid
•Visible epigastric pulsations
•No engorged veins/scars/sinuses
•Soft , non tender
•No organomegaly
•Tympanic node heard all over the abdomen
•Bowel sounds present
CENTRAL NERVOUS SYSTEM:
•HMF - Intact
•Speech – Normal
•No Signs of Meningeal irritation
•Motor and sensory system – Normal
•Reflexes – Normal
•Cranial Nerves – Intact
•Gait – Normal
•Cerebellum – Normal
•GCS Score – 15/15
PROVISIONAL DIAGNOSIS :
HEART FAILURE
RIGHT SIDED PLEURAL EFFUSION
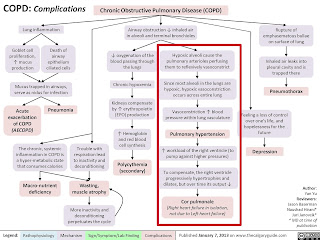
COPD
LEFT LOWER LIMB CELLULITIS
INVESTIGATIONS:
Investigations on 1/7/21:
CHEST X-RAY

LIVER FUNCTION TEST
SERUM CREATININE
BLOOD UREA
SERUM ELECTROLYTE
HEMOGRAM
COMPLETE URINE EXAMINATION
2D ECHO
ECG
FINAL DIAGNOSIS:
HFrEF ? 2° to CAD
B/l PLEURAL EFFUSION (R > L)
AKI ( ? prerenal ) CRS -1
ALCOHOLIC LIVER DISEASE
COPD
LEFT LOWER LIMB CELLULITIS
Investigation on 3/7/21:
ECG: ATRIAL FIBRILLATION, Irregular RR interval, No P wave
Investigations on 5/7/21:
ECG
HEMOGRAM
BLOOD UREA
SERUM CREATININE
SERUM ELECTROLYTES
Investigation on 7/7/21:
TREATMENT :
Treatment on 2/7/21 :
1) Fluid restriction <1lit/day
2) Salt restriction. <2gm/day
3) Inj. Ceftriaxone 1gm IV/BD
4) Tab LASIX 40mg BD (8am to 4pm)
5) Tab MET-XL 25mg BD
6) Tab ECOSPIRIN-AV 75/20 mg OD
7) BP PR temp and spO2 monitoring
Treatment on 3/7/21 :
1) Fluid restriction <1lit/day
2) Salt restriction. <2gm/day
3) Inj. Ceftriaxone 1gm IV/BD
4) Tab LASIX 40mg BD (8am to 4pm)
5) Tab MET-XL 25mg BD
6) Tab ECOSPIRIN-AV 75/20 mg OD
7) BP PR temp and spO2 monitoring
Treatment on 4/7/21:
1) Fluid restriction <1lit/day
2) Salt restriction. <2gm/day
3) Inj. Ceftriaxone 1gm IV/BD
4) Tab LASIX 40mg BD (8am to 4pm)
5) Tab MET-XL 25mg BD
6) Tab ECOSPIRIN-AV 75/20 mg OD
7) Inj. CLINDAMYCIN 600mg IV/TID
8) BP PR temp and spO2 monitoring
Treatment on 5/7/21 :
1) Fluid restriction <1lit/day
2) Salt restriction. <2gm/day
3) Inj. Ceftriaxone 1gm IV/BD
4) Tab LASIX 40mg BD (8am to 4pm)
5) Tab MET-XL 25mg BD
6) Tab ECOSPIRIN-AV 75/20 mg OD
7) Tab DIGOXIN 0.25 mg stat
8) Inj. CLINDAMYCIN 600mg IV/TID
9) BP PR temp and spO2 monitoring
Treatment on 6/7/21 :
1) Fluid restriction <1lit/day
2) Salt restriction. <2gm/day
3) Inj. Ceftriaxone 1gm IV/BD
4) Tab LASIX 40mg BD (8am to 4pm)
5) Tab MET-XL 25mg BD
6) Tab ECOSPIRIN-AV 75/20 mg OD
7) Tab DIGOXIN 0.25 mg OD
8) Inj. CLINDAMYCIN 600mg IV/TID
9) BP PR temp and spO2 monitoring
Treatment on 7/7/21 :
1) Fluid restriction <1lit/day
2) Salt restriction. <2gm/day
3) Inj. Ceftriaxone 1gm IV/BD
4) Tab LASIX 40mg BD (8am to 4pm)
5) Tab MET-XL 25mg BD
6) Tab ECOSPIRIN-AV 75/20 mg OD
7) Tab DIGOXIN 0.25 mg OD
8) Inj. CLINDAMYCIN 600mg IV/TID
9) BP PR temp and spO2 monitoring
Patient improved symptomatically and was discharged in a hemodynamically stable condition.
NEXT ADMISSION:




















Comments
Post a Comment